ISSN: 2319-9865
ISSN: 2319-9865
Kashinatha Shenoy M1*, Gopalakrishna K2 and Preetha1
1Department of Ophthalmology, Malabar Medical College and Research Centre, Modakkalur, Atholi, Calicut, India
2Department of Anatomy, Malabar Medical College and Research Centre, Modakkalur, Atholi, Calicut, India
Received: 22 August 2013 Accepted: 10 September 2013
Visit for more related articles at Research & Reviews: Journal of Medical and Health Sciences
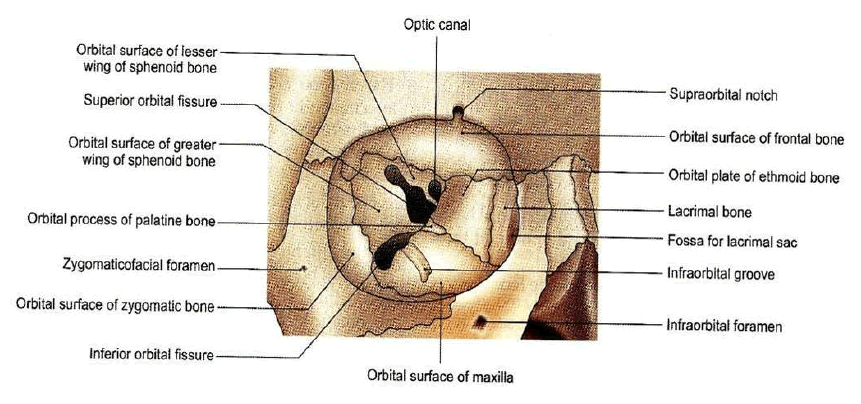
The orbits are boney cavities lodging the eyeballs, extraoccular muscles, nerves, blood vessels and lacrimal gland. Out of 12 pairs of cranial nerves; 2nd, 3rd, 4th, 6th,a part of 5th and some sympathetic fibers are are also present in the orbit. Nature has provided orbit for the safety of the eyeball. The long axis of the each orbit passes backwards and medially. The medial walls are parallel to each other at a distance of 2.5 cms but the lateral walls are set at right angles to each other.
orbit, orbital disease, clinical, cranial nerves
The effect of any disease in the orbit is not only governed by the primary nature of the process but also by the anatomic pattern of involvement.
The patterns of anatomic involvement can be divided into anterior, diffuse, apical, myopathic, ocular, intraconal, optic nerve, periorbital and lacrimal drainage system.
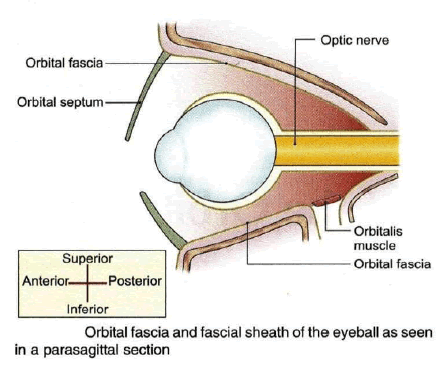
The orbit is a pear shaped cavity, the stalk of which is the optic canal. The intra orbital portion of the optic nerve is longer [25mm] than the distance between the back of globe and the optic canal [18mm].this allows for significant forward displacement of the globe [Proptosis] without excessive stretching of optic nerve.
Consists of two bones: wing of the sphenoid none and orbital plate of frontal bone. It is located adjacent to anterior cranial fossa and the frontal sinus. A defect in the orbital roof may cause pulsatile proptosis as a result of transmission of cerebrospinal fluid pulsation to the orbit.
Relations
• Above, it is related to frontal lobe cerebrum and meninges.
• Below, it is related to frontal nerve, levator palpebrae superioris, superior rectus, superior oblique trochlear nerve and lacrimal gland.
Clinical applications
As the roof is perforated neither by major nerves nor by blood vessels, it can be easily nibbled away in transfrontal orbitotomy.
It consists of two bones: greater wing of sphenoid, and zygomatic. The anterior half of the globe is vulnerable to lateral trauma since it protrudes beyond the lateral orbital margin.
Relations
• It separates the orbit from temporal fossa and from middle cranial fossa.
• Medially it is related to lateral rectus, lacrimal nerve and vessels and zygomatic nerve.
Clinical applications
The anterior half of globe is not covered by bone on lateral side. Hence, palpation of retrobulbar tumors is easier from the lateral side. It is the strongest portion of the orbit and needs to be sawed open in lateral orbitotomy The zygomatico-sphenoid suture is an important landmark during surgery.
It consists of three bones. Zygomatic, maxillary and palatine bone. the posteromedial portion of the maxillary bone is relatively weak and may be involved in a blowout fracture. The orbital floor also forms the roof of the maxillary sinus so that maxillarycarcinoma invading the orbit may displace the globe upwards.
Relations
• Below it is related to maxillary air sinus.
• Above it is related to inferior rectus muscle, inferior oblique muscle and nerve to inferior oblique.
Clinical applications
The orbital floor being quite thin is commonly involved in ‘blow –out fractures’ and is easily invaded by tumors of the maxillary antrum.
It consists of four bones:maxillary,lacrimal,ethmoid, and sphenoid. The lamina papyracea, which forms the part of medial wall, is paper thin and perforated by numerous foramina for nerves and blod vessels. Orbital cellulitis is therefore frequently secondary to ethmoidal sinusitis.
Relations
• Medial to the medial wall lie anterior ethmoidal air sinuses, middle meatus of nose, middle and posterior ethmoidal sinuses and sphenoidal air sinuses.
• The orbital surface of medial wall is related to superior oblique muscle and medial rectus muscle. In between the two muscles lie anterior ethmoidal nerve, posterior ethmoidal nerve, infra trochlear nerve, terminal branch of ophthalmic artery.
Clinical applications
It is the thinnest wall of the orbit. This accounts for ethmoiditis being the most common cause of orbital cellulites, especially in children. The medial wall is frequently eroded by inflammatory lesions, cysts and neoplasms.
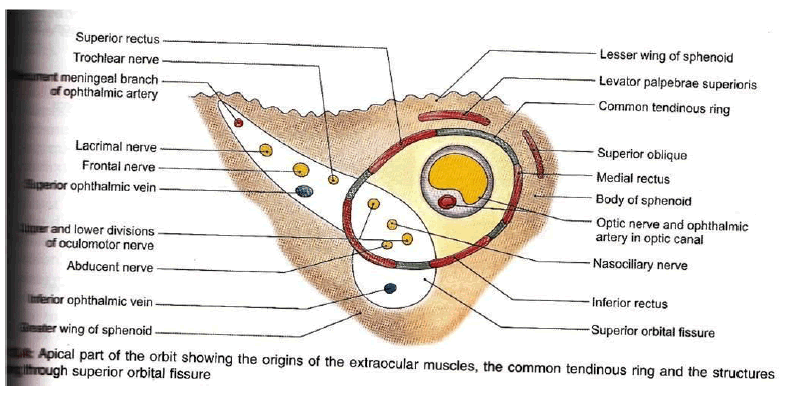
The superior orbital fissure is a slit linking the cranium and orbit, between the greater and lesser wings of sphenoid bone, through which pass the following important structures.
The superior portion contains lacrimal, frontal and trochlear nerves, and and the superior ophthalmic vein. The inferior portion contains superior and inferior divisions of the occulomotar nerve, abducens and nasociliary nerves and sympathetic fibres from cavernous plexus.
Inflammation of the superior orbital fissure and apex [Tolosa-Hunt syndrome] may therefore result in a multitude of sign including ophthalmoplegia and venous outflow obstruction.
The inferior orbital fissure lies between the greater wing of sphenoid bone and maxilla, connecting the orbit to the pterygopalatine and infratemporal fossae. Through it run the maxillary nerve, the zygomatic nerve and branches of the pterygopalatine ganglion, as well as the inferior ophthalmic vein.
The orbit is divisible into a number of spaces. Knowledge of the main compartments of the orbit and their boundaries helps in choosing the most direct approach to the tumor.
This is a potential space between orbital bones and the periorbita. Dermoid cyst, epidermoid cyst, mucocele, subperiosteal abscess, myeloma, osteomatous tumor, hematoma and fibrous dysplasia are commonly seen in this space.
This space is bounded peripherally by periorbita, internally by the four extra ocular muscles, anteriorly by the septum orbitable. Posteriorly, it merges with the central soace. Tumors present in this space produce eccentric proptosis and can usually be palpated. Common tumors present in this space are malignant lymphoma, capillary hemangioma, neoplasms of the lacrimal gland and pseudotumors. Tumors residing in this space are explored mostly by anterior orbitotomy.
It is also called muscular cone or posterior or retrobulbar space. Contents of this space include optic nerve and its meninges, superior and inferior divisions of oculomotor nerve, abducent nerve, nasociliary nerve, ciliary ganglion, ophthalmic artery, superior ophthalmic vein and central orbital fat. Many of the circumscribed orbital tumors such as cavernous hemangioma, solitary neurofibroma, meningioma, optic nerve glioma occur in this space and usually produce axial proptosis. Such tumors are aften removed through a lateral orbitotomy.
It is a potential space around the eyeball between the sclera and tenon’s space. Pus collected in this space is drained by incision of tenon’s capsule through the conjunctiva.
It is bounded peripherally by periorbita; anteriorly becoming continuous with the anterior and central spaces.
Axial and coronal views are complementary for showing bony and soft tissue anatomy. The axial view is superior for demonstrating the lateral and medical bony margins, the superior orbital fissure, and the optic canal. Coronal views are best for assessing the floor and roof. The lacrimal sac and nasolacrimal duct as well as the inferior orbital fissure and infraorbital canal are equally seen on axial or coronal images.
• Orbital Trauma.
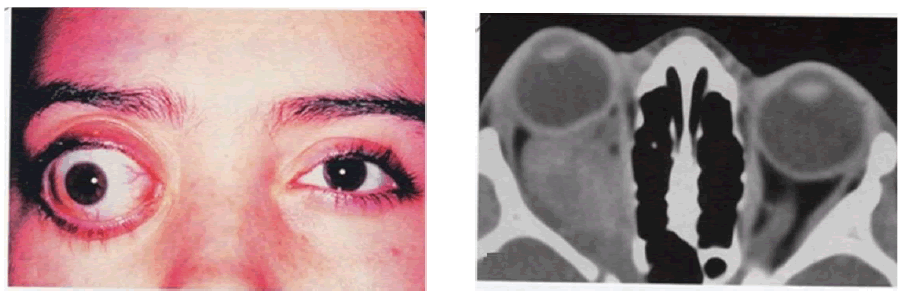
• Evaluation of extraocular muscles thyoid eye disease.
• Bony involvement of orbital tumors.
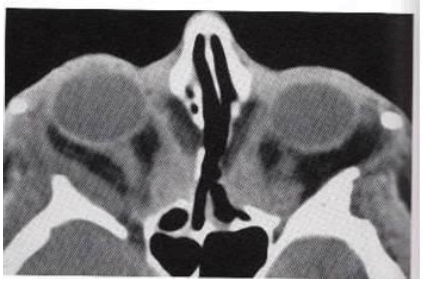
• Orbital cellulitis
• Detection of intraorbital calcification.
• Detection of acute cerebral haemorrhage.
• Thyroid Eye Disease
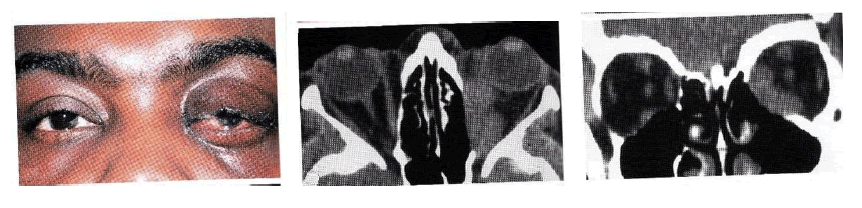
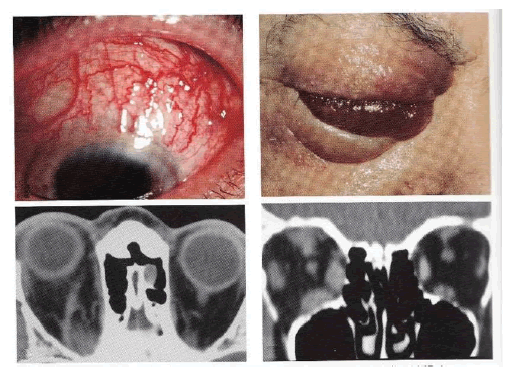
• Infections: Preseptal cellulitis, Orbital cellulitis, Rhino-orbitalmucormycosis
• Non Infective Inflammatory disease: Orbital myositis, Acute dacryoadenitis, Tolosa- hunt syndrome.
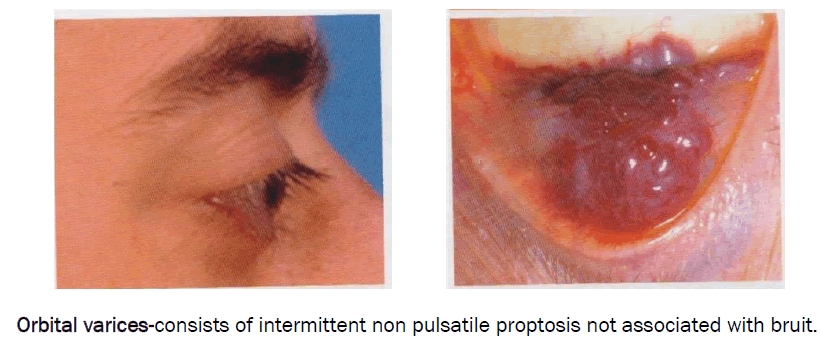
• Vascular Malformation: Lymhangioma, Varices.
• Carotid cavernous fistula Direct/ indirect
• Cystic lesions: Dacryops, dermoid cyst
• Tumors: Capillary and cavernous haemangioma, Optic nerve glioma, Optic nerve sheath meningioma
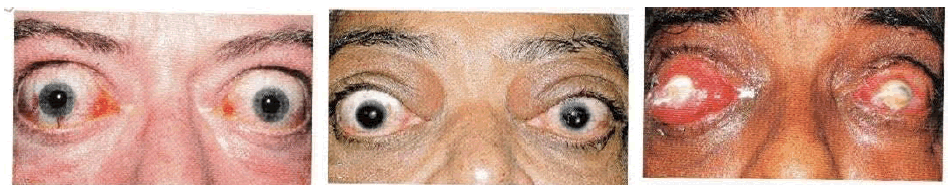
Thyroid opthalmopathy is an organ specific auto immune disease. TED[ Thyroid eye disease ] has five main clinical manifestation, 1.soft tissue involment 2. Lid retraction 3.proptosis 4. Optic neuropathy 5.restrictive myopathy.
CT Scan findings- CT Scan shows muscle enlargement and not involving tendons
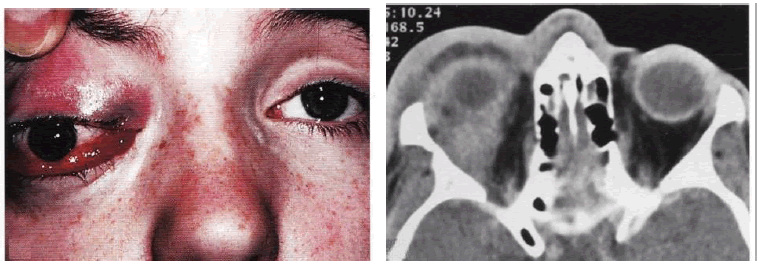
It can be classified on the basis of a] etiology-spontaneous and traumatic fistulas b] haemodynamics –high and low flow c. anatomy- [direct and indirect] fistula. Trauma is responsible for 75% of the cases.
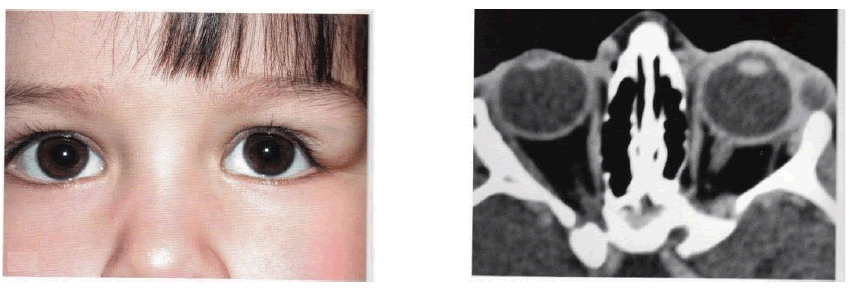
Dermoids are lined by keratinized stratifiefd squamous epithelium and sub cutaneous location along embryonic line of closure. Dermoids may be a] superficial b] deep, located anterior or posterior to the orbital septum respectively.
The majority is isolated lesions, but a significant arise within the context of neurofibromatosis. Bilaterality is pathognomonic for Von Recklinghausen’s disease. There is female predominance, with 75% occurring in the first decade of life. The clinical character can be best understood by dividing into orbital, orbito cranial, chiasmal and diffuse type.
Orbital glioma arise within the orbit where they are characterized by proptosis (frequently non axial) and visual loss.
CT-Orbital type presents as enlarged fusiform optic nerve with smooth intact dural margins. Anterior kinks adjacent to the globe and low density cystic areas are frequent and characteristic, reflecting pliability of the nerve and focal areas of degeneration within the tumor.

They frequently lead to visual loss; those confined to and arising from the optic nerve sheath cause unilateral deterioration, whereas those arising intracranially often affect vision bilaterally.
• Intracranial Meningioma
• Optic canal meningioma
• Optic nerve meningioma
The major sites affecting the orbital and visual structures are the sphenoid ridge, suprasellar area and olfactory groove. The medial tumors cause cranial nerve palsies, visual deficits and venous obstruction. Remote tumors exert their effect by virtue of raised intracranial pressure or mass effect.
Intracranial – lesion is well defined, homogenous and characteristically of increased density with uniform enhancement post contrast infusion. Optic nerve meningioma generally demomstrates one of the three radiologic patterns: diffuse thickening, fusiform swelling anterior or posterior globular enlargement and nodular type. There is a pathognomonic subgroup characterized by calcification and railroad tracking [7,8]
Authors wish to clarify that they have not received any financial support or funding from any commercial sources.