ISSN: 2319-9865
ISSN: 2319-9865
Department of Midwifery, Harar Health Science College, Harar, Ethiopia
Received date: 26/02/2019; Accepted date : 01/04/2019; Published date: 08/04/2019
Visit for more related articles at Research & Reviews: Journal of Medical and Health Sciences
Background: Occupational health hazard is a dangerous phenomenon, substance, human activity or condition that may cause loss of life injury or other health impacts at the workplace and it is an injury sustained from falls, needle pricks and contact with infected body fluids from patients, long periods of standing due to job demands, lifting heavy patients and objects. Yearly over 2 million people worldwide die of occupational injuries & work related diseases. Among 35 million health care workers worldwide; about 3 million are also exposed to blood borne pathogens yearly.
Objective: To assess safety measures practice among health care workers in Jugol Hospital, Harari region, Eastern Ethiopia, 2018.
Materials and Methods: Facility based cross sectional study by using self- administered questionnaire was conducted. Data were collected among randomly selected 150 health care workers from different wards by using Stratified random sampling technique. Ethical clearance was obtained from HHSC ethical review committee. Informed consent also obtained from respondents. Data was entry & analysis was performed using SPSS version 21. Result was presented in tables and graphs.
Results: The overall prevalence of occupational hazards was 89(60.1%). Majority 86 (58.1%) and 78 (52.7%) were exposed to Physical and Biological hazards while 47 (31.8%) and 51 (34.5%) were suffered by Chemical & Ergonomic hazards. More than half (73.6) were not washing their hand. While 57.4% did not Wearing gown at work place.
Conclusions & Recommendation: Generally there is great risk to occupational hazard. The major challenges are absence and dissemination of written occupational health and safety measure policies for each department and ward, safety committee, organized time of training on safety rules and inadequate provision of personal protective equipment there for the Hospital need adopt occupational health and safety policy.
Occupational hazards, Safety measures, Health care worker
An occupational health hazard is a dangerous phenomenon, substance, human activity or condition that may cause loss of life, injury or other health impacts at the workplace and it is an injury sustained from falls, long periods of standing due to job demands, lifting heavy patients and objects needle pricks and contact with infected body fluids from patients [1]. Health care workers are potentially exposed to infectious materials and frequently exposed to occupational hazards through per cutaneous injury such as needle stick or cut with sharps blood, tissue, specific body fluids, medical supplies, equipment or environmental surfaces contaminated with these substances [2,3]. Occupational hazards are mostly under reported due to inadequate research [4,5]. Global health workers reported the greatest number of needle stick injuries occurs among nurses followed by laboratory workers and physicians [6].
Statement of the problem: Yearly over 2 million people worldwide die of occupational injuries and work related diseases [7]. Each year among 35 million health care workers worldwide; about 3 million are exposed to blood borne pathogens through per cutaneous route due to occupational accidents [8]. The International Labor Organization (ILO) estimates that over 350,000 casualties and over 2 million work related deaths each year all attributable to occupational hazards [9]. Occupational Safety and Health Administration (OSHA, 2012) estimates that 5.6 million health care workers working in health care institutions are at high risk of exposure to blood borne pathogens including; HIV,HBV,HCV and other potentially infectious materials [10]. In sub- Saharan Africa the fatality rate per 100,000 health care workers is 21 and the accident rate 16,000.This means that each year 54,000 workers die and 42 million work related accident take place that cause at least 3 days absence from work [11]. Ethiopia is categorized among under developed countries and do not have much data on health and safety. Assessment made by federal civil service agency describes in 2008 G.C that 14 males and 8 females died, 7 males and 8 females discharged from work due to disability and 6 males and 27 females transferred to other jobs due to various work place injuries [12].
Significance of the study: There is no sufficient data in the study area regarding the topics there for the finding of this study will be helpful to provide the regional Health office, Hospital administration and other stakeholders and for health care workers with valuable information to design appropriate targeted innervations that will effectively address the problem of occupational hazards. The study will provide information for health care workers to prevent themselves from occupational hazards and also it will be used as baseline data for other researchers.
General objective: Assessment of occupational hazards and safety measures among health care workers in Jugol hospital, Harari region, Eastern Ethiopia 2018 G.C.
Specific objective:
1. To assess occupational hazard exposures among health care workers in Jugol hospital, Harari region, eastern Ethiopia2018 G.C.
2. To assess safety measures practice among health care workers in Jugol hospital, Harari region, eastern Ethiopia.
Study area and study period: The study was conducted in Jugol hospital Eastern Ethiopia, which was found in Harar Region 526 kilometer far from the capital city of Ethiopia. It is a regional Hospital which was established in 1902 G.C and it provide serves for more than for 500,000 populations. In the hospital 355 staffs (211 qualified health care workers and 144 supportive staffs) 125 beds and 20 different wards was available. The study was conducted from January 12-26, 2018 G.C.
Study design: Facility based cross sectional study was employed.
Source population: All health care workers in Jugol.
Study population: Data were collected from randomly selected 150 Health care workers from different ward.
Sample size: Sample size was determined by using single population proportion formula with the prevalence of occupationally exposed health care workers 47% by research done at Jimma 5% marginal error and 95% confidence level [13]. Where z stands for normal variable confidence interval 95%=1.96.
p=prevalence (47%) (44)
q=1-p=1-0.47=0.53
n=the desired sample size
d=the margin of sampling error (5%)
Therefore, using the formula n become,
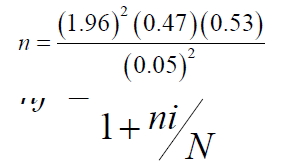
n=382
Correction formula was used to reduce the sample size,
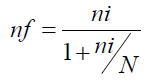
nf= final sample size
ni =standard sample size
N= total sample taken
So we use this formula due to our total population is less than 10,000.
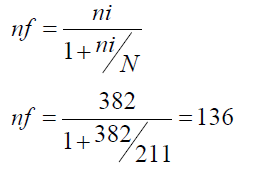
By adding 10% of sample size for non-response rate,
136+14=150
nf=150 so the final sample size becomes 150
Sampling techniques: The sample was proportionally allocated for different wards based on the number of available functional staffs (Figure 1).
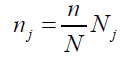
Where; nj is sample size of the jth stratum
Nj is population size of the jth stratum
n = n1 + n2 + ...+ nk is the total sample size
N = N1 + N2 + ...+ Nk is the total population size
Dependent variables: Occupational hazards and safety measure Independent variable - Socio demographic (Age, Sex, Educational status, Professional status) Work experience, Training taken.
Data collection tolls & method: Before actual data collection, the questionnaire was prepared in English version and Interview was conducted.
Data quality assurance: To assure the quality of the data, properly design data collection instrument was developed and pre-tested in 5% of Health Care Workers was done in Hiwot Fana Specialized University Hospital and Correction was done based on the findings. Training was given for data collector’s supervisor and data entry clerks prior to the study. The collected data were reviewed for completeness, consistency and legibility on daily based. Supervision was frequently made by 4 supervisors together with the principal investigator.
Data processing and analysis: Epi-Data version 3.1 and SPSS version 21 were used for data entry and analysis. The univariate analysis such as proportions, percentages, ratios, frequency distributions and appropriate graphic presentations as well as measures of central tendency and measures of dispersion were made. Data was presented in frequency, percentages, tables and graphs.
Ethical consideration: Ethical clearance was obtained from Harar Health Science College Ethical Review Committee before conducting the research. Permission was obtained from study institution. All the participants were informed the purpose, advantages and disadvantages, and their right to be involved or not. Informed consent was obtained from study participants. Confidentiality was maintained by avoiding names and other personal identification.
Biological hazards: Are hazards caused when blood, Splash and other body fluid contact with individual’s body.
Chemical hazard: Injury due to chemical substance.
Ergonomic hazard: Harm or injury due to work position.
Occupational hazard: Harm or injury and any damage due to work.
Physical hazard: Is a damage or injury on physical part of health care worker.
Psychological hazard: Is a mental hazard due to stress, discomfort and work dissatisfaction.
Socio demographic characteristics of the respondents: From 150 study participant 148 healths professional were interviewed which makes response rate 98.7%. Half of the respondent 74 (50%) were male and majority of the respondent were between the age group 26-35 (54.7%) with mean age of 32.14 and standard deviation of (SD ± 9.665).Pertaining to professional qualifications majority and the least number of study participants were nurses 90 (60.8%) and health officers 1 (0.7%) (Table 1).
| S .No | Variable | Characteristics | Number | Percentage |
|---|---|---|---|---|
| 1 | Age (year) | <25 | 31 | 21 |
| 26-35 | 81 | 54.7 | ||
| 36-45 | 16 | 10.8 | ||
| 46-55 | 12 | 8.1 | ||
| >56 | 8 | 5.4 | ||
| 2 | Sex | Male | 74 | 50 |
| Female | 74 | 50 | ||
| 3 | Religion | Orthodox | 68 | 45.9 |
| Protestant | 16 | 10.8 | ||
| Muslim | 63 | 42.6 | ||
| Other | 1 | 0.7 | ||
| 4 | 31 Marital status | Single | 62 | 41.9 |
| Married | 82 | 55.4 | ||
| Divorced | 3 | 2.0 | ||
| Widowed | 1 | 0.7 | ||
| 5 | Professional status | Physician | 22 | 14.9 |
| Nurse | 90 | 60.8 | ||
| Pharmacy | 12 | 8.1 | ||
| Medical Lab | 14 | 9.5 | ||
| Radiographer and radiologist | 3 | 2.0 | ||
| Health officer | 1 | 0.7 | ||
| Anesthesia | 6 | 4 |
Table 1: Socio demographic characteristic of health care workers in Jugol hospital, 2018.
Occupational hazards: The Overall prevalence of occupational hazard on this study was 89 (60.1%), among this: physical hazard 86 (58.1%), biological hazard 78 (52.7%), psychological 75 (50.7%), Ergonomic hazard 51 (34.5%) and Chemical hazard 47 (31.8%) accounts respectively.
Respondents were stated different reason for having accidents. 45 professional were because of low provision of adequate protective clothing and equipment, 26 due to of lack of training on occupational hazard and safety measure and 31 were due to ignorance on health and safety matters. 3 of health care workers develop Pulmonary TB because of the exposure to respiratory secretion, 11 of them exposed to other health problems like fungal skin infection, respiratory infection and others, but they do not have the history of HIV, HBV and HCV because of exposure.
Biological hazards: Regarding biological the highest and the least exposure were blood 51 (34.5%) and infected skin lesion 8 (5.4%) (Table 2).
| S .No | Biological hazard | Exposure status | |||
|---|---|---|---|---|---|
| Yes | No | ||||
| Number | Percent | Number | Percent | ||
| 1 | Blood | 51 | 34.5 | 97 | 65.5 |
| 2 | Body Fluid | 33 | 22.3 | 115 | 77.7 |
| 3 | Respiratory secretion | 14 | 9.5 | 134 | 90.5 |
| 4 | Infected skin lesion | 8 | 5.4 | 140 | 94.6 |
| 5 | Urine/stool | 18 | 12.2 | 130 | 87.8 |
Table 2: Exposure of Biological Hazard in Jugol hospital among health care workers, 2018.
Physical Hazard: Among different type of physical hazard the most common one were sharp material related injury 80 (54.1%) followed by cut and wound 21 (14.2%) (Table 3).
| S .No | Physical hazard | Exposure status | |||
|---|---|---|---|---|---|
| Yes | No | ||||
| Number | Percent | Number | Percent | ||
| 1 | Physical Hazard | 86 | 58.1 | 62 | 41.9 |
| 2 | Sharp material related injury | 80 | 54.1 | 68 | 45.9 |
| 3 | Cut and wound | 21 | 14.2 | 115 | 77.7 |
| 4 | Broken bone or fracture | 4 | 2.7 | 134 | 90.5 |
| 5 | Burn | 2 | 1.4 | 140 | 94.6 |
Table 3: Exposure of physical Hazard in Jugol hospital among health care workers, 2018.
Chemical hazards: The most common physical hazard was exposed to disinfectants 15.5% and the least exposure was contact with sterilizing agents.
Ergonomic hazard: Of 148 study participants 57 (38.5%) of health care workers were suffered from ergonomic hazards, due to sprain and strain, visualizing, sitting and standing for long period of time while the rest 91 (61.5%) where had not (Figure 2).
Psychological hazard: Out of 148 study participants interviewed on current occupational health and safety measures majority of health workers were 58 (39.19%) dissatisfied (Figure 3).
Concerning personal practices of health care workers, Most of them do not wash their hands before and after visit of each patient. Almost half of the health care workers were eating habits at work place and they wear gown in rest room also. Majority of the health work 101 (68.2%) were wear gown while the least utilized personal protective materials were boots 12 (8.1%) (Table 4).
| S. No | Health Workers Practice | Yes | No | ||
| Number | Percent | Number | Percent | ||
| 1 | Eating habit at work place | 73 | 49.4 | 75 | 50.6 |
| 2 | Washing hand before and after caring for patient | 39 | 26.4 | 109 | 73.6 |
| 3 | Wearing gown in rest rooms | 79 | 53.4 | 69 | 46.6 |
| 4 | Wearing gown in lounge rooms | 6 | 4.1 | 142 | 95.9 |
| 5 | Wearing gown at work place | 63 | 42.6 | 85 | 57.4 |
| Personal protective usage | Yes | No | |||
| Number | Percent | Number | Percent | ||
| 1 | Cape | 13 | 8.8 | 135 | 91.2 |
| 2 | Goggle | 14 | 9.5 | 134 | 90.5 |
| 3 | Mask | 45 | 30.4 | 103 | 69.6 |
| 4 | Gown | 101 | 68.2 | 47 | 31.8 |
| 5 | Glove | 90 | 60.8 | 58 | 39.2 |
| 6 | Apron | 14 | 9.5 | 134 | 90.5 |
| 7 | Boot | 12 | 8.1 | 136 | 91.9 |
Table 4. Personal practices and personal protective equipments usage of health care workers at Jugol hospital, 2018.
In this study the prevalence of physical hazards and ergonomic hazards were 58.1% and 34.5% which was nearly similar with research finding in Jimma University Medical Center which was physical hazards (57.6%) and ergonomic hazards (31.5%) [13]. But our finding is higher when compared with study conducted in Adiss Abebab which was Physical hazards 17.11% and Ergonomic hazards 24.58%. This difference might be due to difference in study area as well as work over load on the staffs in our study [14].
On this study large number of health care workers 80 (54.1%) reported as they had been exposed for needle stick injuries and nurses were the most frequent victims for needle stick/sharp object injuries. This finding was greater than the result found in study conducted on Army force Referral and teaching hospital, Addis Ababa and South nation nationalities and people region which was 26.6% and 32.4% had sustained needle stick injuries respectively [15]. This might be due to because not having training on occupation health and safety measures.
In this study 39 (26.4%) participants had experience of hand washing practice after end of their routine activities or following direct contact of patient all the time which was less than the study conducted at Addis Ababa (53.2%) [16]. This difference might be due to lack of availability of enough hand washing facility and water.
In general, the study result showed that in Jugol Hospital Health care workers were exposed to different occupational hazards. Majority of the health workers were exposed for blood contact 51 (34.5%) Sharp material related injury 80 (54.1) and disinfectants, 13 (8.8%) splash. Almost half 58 (39.19%) of the respondent were not satisfied regarding organization occupational health and safety measures.
Jugel hospital need to:
• To establish occupational health and safety committee.
• To provide infection prevention training.
• To reduce work load.
• To supply adequate amount of PPE.
Harari regional health office:
• To adopt occupational health and safety policy and disseminate.
• To employ health care workers to reduce work load.
• To provide training for health care workers and concerning bodies on occupational health and safety.
• To conduct further research on this topic.
The questioner was pretested on similar setting and a necessary modification was made.
The study was using combined both qualitative and quantitative methods.
The study was limited to Jugol Hospital only and the results cannot be generalized to all Harari hospitals and health services. As it was a cross sectional study it’s impossible to make causal reference for population under investigation.