ISSN: 2319-9865
ISSN: 2319-9865
Mukesh I Shukla, Ajay Rathod, Swathi N*, Jayesh Kamat, Pramod Sarwa, and Vishal Divecha
Department of Anaesthesia, BJMC, Ahmedabad, Gujarat, India.
Received: 27 March 2013 Accepted: 10 May 2013
Visit for more related articles at Research & Reviews: Journal of Medical and Health Sciences
To evaluate the effectiveness of epidural administration of two different doses of clonidine for postoperative pain relief and its side effects. Study was conducted in 50 patients scheduled for different surgeries under anaesthesia. The patients were randomly divided into two groups. Group I received 150 μg clonidine and Group II received 100 μg clonidine and subsequent doses of 75 μg in 10 ml normal saline. Identical epidural anaesthesia procedures were used for both groups. Onset and duration of action of epidural clonidine, analgesia (VAS score), heart rate, blood pressure and Ramsay sedation score at regular intervals were monitored. The mean duration of post operative analgesia was 457.4±20.57 minutes in Group I as compared to 428.4±22.11 minutes in Group II. A fall in pulse rate and mean blood pressure was observed at 1 hour, more in Group I as compared to Group II of epidural clonidine. No further fall was observed after 1 hour. The sedation scores between the two groups were comparable. Clonidine significantly leads to rapid onset of analgesia and prolongs the duration of postoperative analgesia and reduces postoperative analgesic consumption with initial bolus dose 150μg as compared to 100μg.
Clonidine, Epidural, Postoperative analgesia.
The International Association for the study of pain defines pain as "an unpleasant, sensory and emotional experience associated with actual or potential tissue damage or described in terms of such damage”.[1]
Pain relief is one of the important functions of an anaesthesiologist. The technical skills & pharmacological knowledge required to treat pain during surgery place them in an ideal position to do so in the postoperative period. Any method of postoperative analgesia must meet basic criteria such as it must be safe, effective and feasible.
Epidural analgesia was initially limited to the use of local anaesthetic for the provision of postoperative pain relief. Description of spinal opiate mechanisms of analgesia has led rapidly to the widespread use of epidural and intrathecal opioids administration in the treatment of acute and chronic pain syndromes. Unfortunately, opioids produce side effects and the patients may develop tolerance to their analgesic effects2. In addition to opiate mechanisms, other spinal mechanisms and receptor specific agents exist which produce analgesia in animals and humans, when injected in epidural or intrathecal space. Clonidine, an alpha2 adrenergic agonist used in oral form primarily for treatment of hypertension, produces analgesia when applied near the spinal cord.
• To evaluate the effectiveness of epidural administration of two different doses of clonidine 100μg and 150μg for postoperative pain relief.
• To study the effect of clonidine on onset and duration of epidural analgesia.
• To study the sedative and hemodynamic effects of clonidine in epidural analgesia.
The present study was conducted in 50 patients divided in 2 groups of 25 each, scheduled for variety of surgeries.
Detailed preoperative assessment was carried out a day before operation. History of any past or present illness relevant to anaesthesia was obtained. A detailed general as well as systemic examination was done. The patients were explained about the nature and purpose of the study during the preoperative visit. Patients were reassured and informed consent was obtained.
Age: 18-60 years
ASA: I and II
Surgery: Lower abdominal surgery like abdominal hysterectomy, Exploratory laparotomy, Total hip and knee replacement, Modified radical mastectomy, etc
Hypertensive patients.
Patients previously taking clonidine.
Pregnant patients.
Skin infection at the site of epidural injection.
Patients with fixed cardiac output status.
Patients having abnormality of CNS and psychotic patients in whom cooperation would not be proper.
Patients on anticoagulants/ bleeding disorders.
Patients refusal.
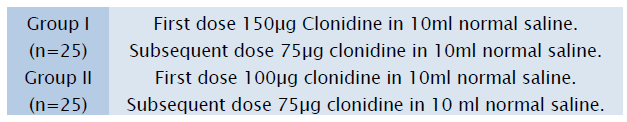
All the patients were randomly divided into 2 groups of 25 patients each.
Epidural analgesia was performed in lateral position via midline approach with the help of Touhy’s epidural needle after taking all aseptic and antiseptic precautions. Epidural space was identified by using “hanging drop method”. After identifying the space epidural catheter was guided upto desired level and catheter was fixed to skin.
Test dose given with Inj.Lignocaine 1% in volume of 10ml given through the epidural catheter to confIrm the epidural space and prevent inadvertent dural puncture. No accidental dural puncture was noted.
After completion of surgery, patient shifted to recovery room, first dose of Inj.Clonidine 150μg (Group 1) or 100μg (Group 2) after diluting in 10ml normal saline given through epidural catheter.
In recovery room patient was observed for Heart Rate, Blood pressure, Respiratory rate, Oxygen saturation every 2 hours for first 24 hour and every 4 hours for next 24 hour. Event of bradycardia and hypotension was noted, treatment given with Inj.Atropine and Inj. Mephentermine accordingly.
Postoperative pain was assessed by visual analogue scale. A 10 cm line is drawn on the paper, and at one end of the line, the patient feels no pain and at the other end is the worse pain ever felt by the patient.
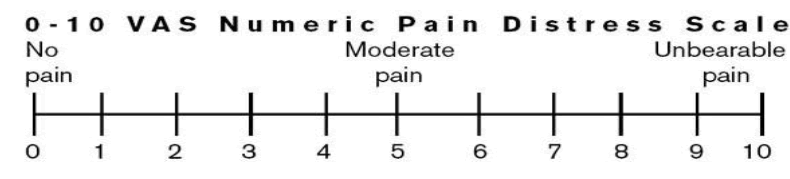
VAS score were recorded every 2 hour onwards till first 24 hours and then every 4 hour for next 24 hour. Subsequent dose of Inj.Clonidine 75μg in 10ml normal saline given in epidural when VAS score >5 for total 48 hours.
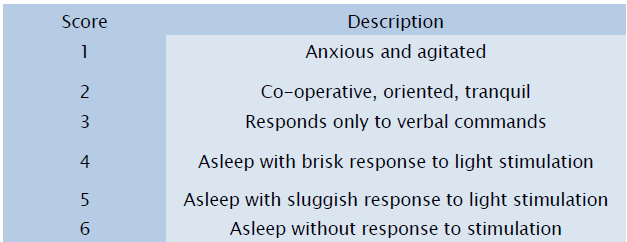
The sedation was assessed by Ramsay scale.
Ramsay Scale
Side effects specifically looked for were
Bradycardia (HR <55 /min)
Hypotension (Systolic blood pressure <30% of baseline)
Dryness of mouth, Fall in respiratory rate( <10 breath/min)
Nausea, Vomiting
Epidural catheter was removed after 48 hours under all aseptic and antiseptic precautions, patency and intact tip of catheter was checked.
The mean age of the patients were comparable in both the groups, being 49.68±16.25 years in Group I and 45.96±16.84 years in Group II.
Statistically no significant difference was observed in sex distribution between the two groups.
The mean time from epidural injection to onset of sensory analgesia was 19.8±3.67 minutes in Group I and 27.8±3.85 minutes in Group II. This difference was statistically significant (p<0.05)
The total duration of analgesia was 457.4±20.57 minutes in Group I and 428.4±22.11 minutes in Group II. This difference was statistically highly significant (p<0.05), indicating a prolongation of analgesia in Group I.
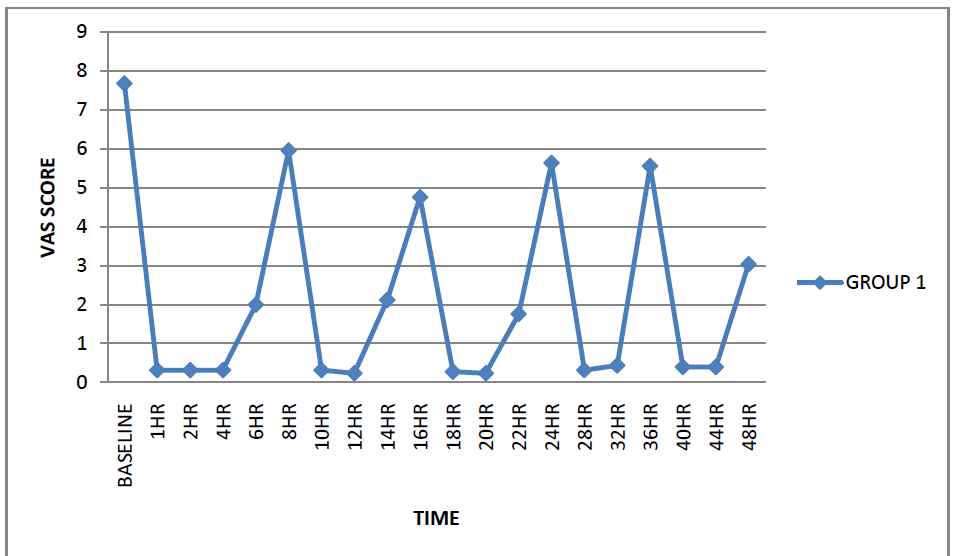

The visual analogue scale scores at 8 hours and 16 hours were statistically significantly lower in Group I as compared to Group II (p<0.05). At the other time intervals, no statistically significant differences were observed between the VAS scores in between the two groups (p>0.05).
Preoperative mean arterial blood pressure was comparable in both the groups. A fall in mean arterial blood pressure started after 45 minutes in both the groups. In Group I, the maximum fall in mean arterial blood pressure (75.36mmHg) as compared to baseline value (95.12mmHg) was 21% which occurred at 1hour after epidural injection. In Group II, the maximum fall in mean arterial blood pressure (78mmHg) as compared to the baseline value (96.56mmHg) was 19% which occurred at 1hour after epidural injection. No patient developed significant hypotension.
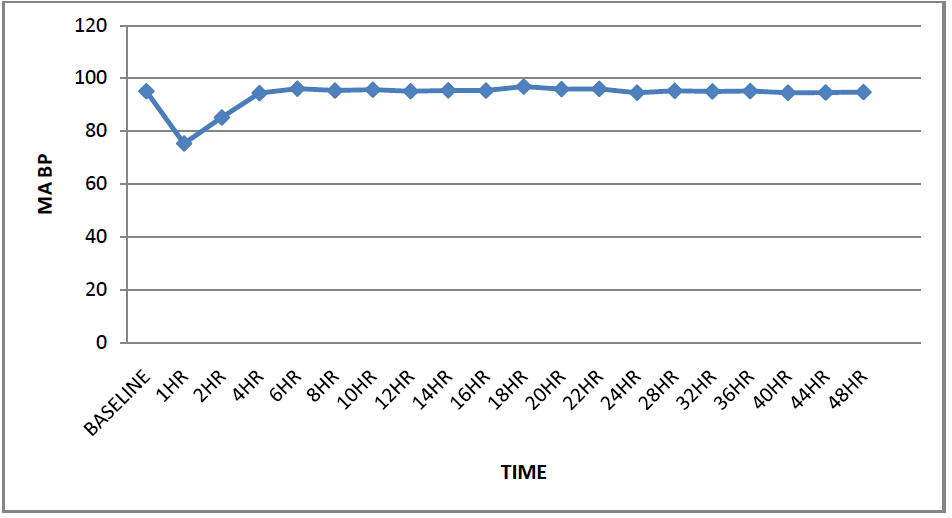
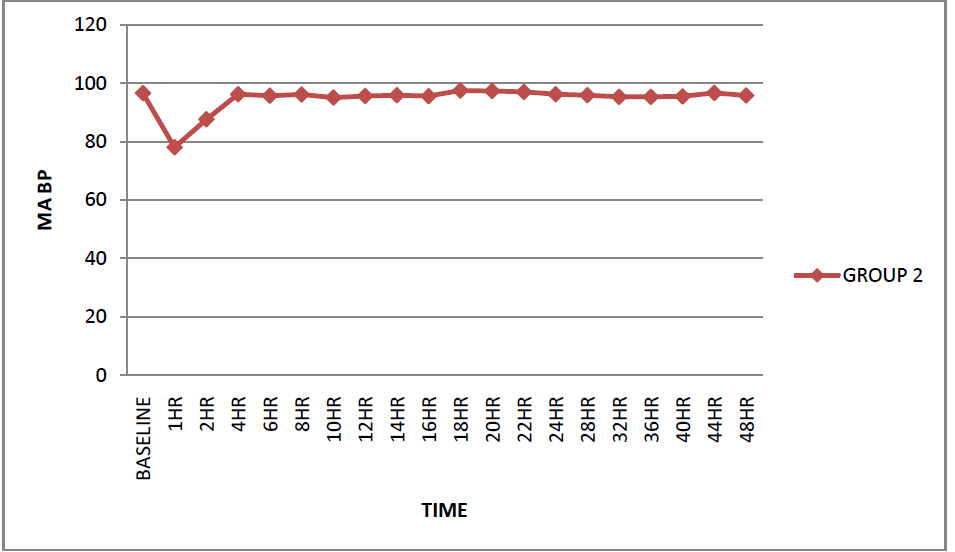
Preoperative mean arterial blood pressure was comparable in both the groups. A fall in mean arterial blood pressure started after 45 minutes in both the groups. In Group I, the maximum fall in mean arterial blood pressure (75.36mmHg) as compared to baseline value (95.12mmHg) was 21% which occurred at 1hour after epidural injection. In Group II, the maximum fall in mean arterial blood pressure (78mmHg) as compared to the baseline value (96.56mmHg) was 19% which occurred at 1hour after epidural injection. No patient developed significant hypotension.
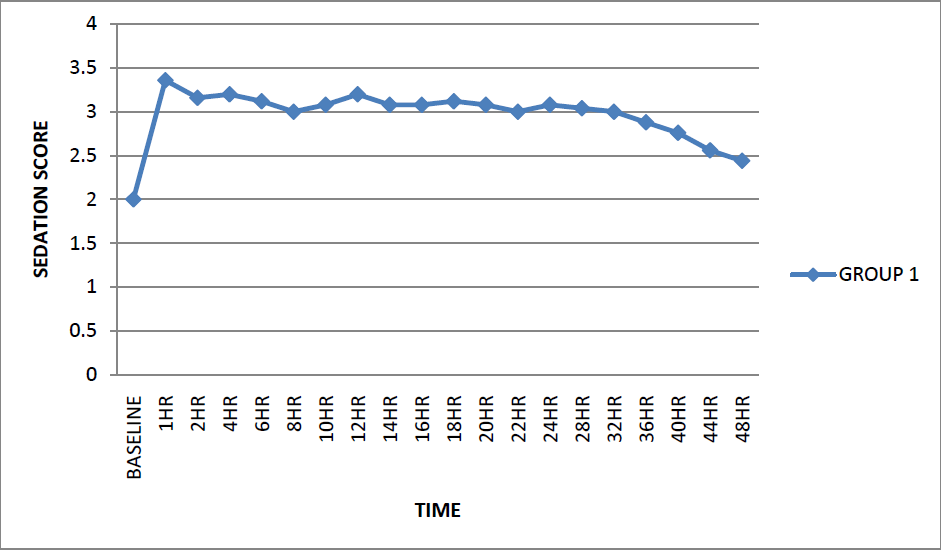
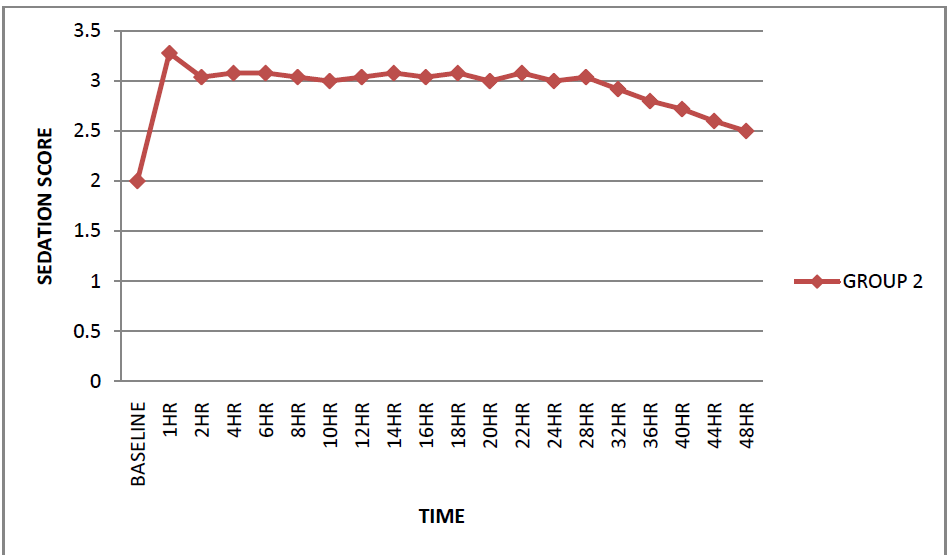
The sedation scores were comparable in both the groups and statistically no significant difference was observed between the two groups. All patients of both the groups show sedation score between 3 and 4.
6 patients developed bradycardia during the postoperative period in Group I, which responded to inj. atropine 0.6 mg given intravenously. Bradycardia was not observed in any patient in Group II. None of the patients had hypotension, fall in respiratory rate, dryness of mouth, nausea and vomiting.
Real art of medicine lies in the treatment of pain. Effective pain control is essential for optimum care of the patients in the postoperative period.
Administration of an analgesic in epidural catheter for surgery has many advantages. There is a high quality monitoring during the early period of the block, provides analgesia for longer duration and attainment of pre-emptive analgesia. This is the reason we choose epidural technique with clonidine as it will provide postoperative analgesia for the operation in a single prick to the patient.
In our study the mean time from epidural injection to onset of analgesia was 19.8±3.67 minutes in Group I and 27.8±3.85 minutes in Group II. This difference was statistically significant (p<0.05). We observed mean duration of analgesia was 457.4±20.57 minutes in Group I as compared to 428.4±22.11 minutes in Group II. This difference was statistically significant (p<0.05). Thus we found that initial larger dose (150 μg) of clonidine is beneficial in prolongation of duration of action, with supplemental equal doses at regular interval as compared to smaller dose (100 μg). We observed that mean VAS was lower in Group I, as compared to Group II at 8 hours and 16 hour which was statistically significant (p<0.05). The mean VAS scores at rest of the study duration were not significantly different (p>0.05) between the two groups at 24 hrs, 36hrs and 48 hrs. We had used a score of more than 5 for analgesic supplementation. After wearing off the effect of clonidine, pain intensity by VAS was higher in group 2 as compared to group 1 throughout 48 post operative hours. The VAS was comparatively low in both the groups of our study on 2nd post operative day as compared to 1st post operative day and it might be due to decreased intensity of surgical incision pain on 2nd post operative day. Thus, clonidine decreases VAS score in a dose dependent manner.
Onset of analgesia is 19.8±3.67 mins in group 1(150 μg) and 27.8 ± 3.85 mins in group 2(100 μg) of our study; mean time of onset of analgesia of our group 1 is comparable with all groups of Eisenach’s4 study, but group 2 onset time is not comparable with them. Thus, clonidine increases the onset of action and the duration of analgesia in a dose dependent manner. VAS also decreases in dose dependent manner.
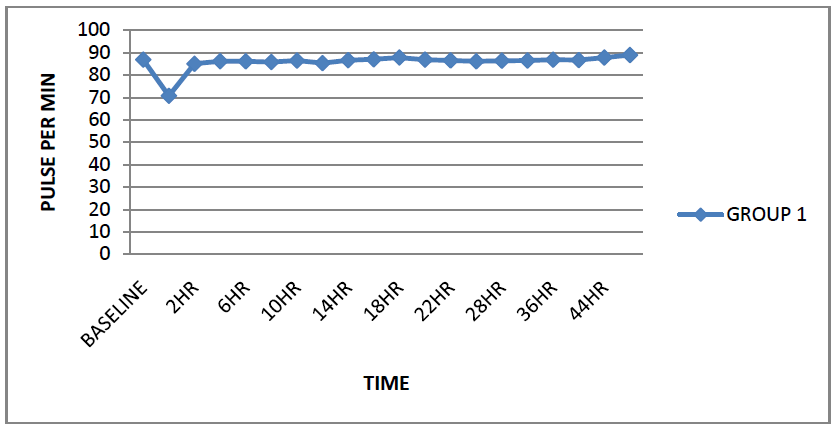
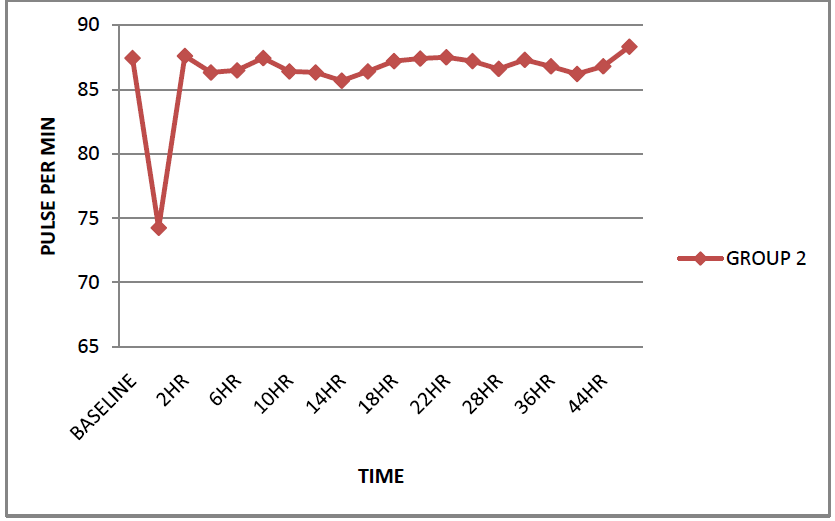
Fall in heart rate was observed after 1hour of epidural injection in both the groups. Maximum fall in pulse rate was seen at 1 hour which is more in group 1(19%) as compare to group 2(15%) which is statistically significant (p<0.05). The difference between the two groups was not statistically significant (p>0.05) after 1 hour in the study period (48 hours). 6 patients in Group I showed fall in heart rate more than 20% during the postoperative period which responded to Inj. Atropine 0.6 mg given intravenously. Maximum changes in heart rate occurred latter than maximum changes in BP and this results is comparable with Yuan-Shiou Huang3 et al and Eisenach JC4 et al studies.
Thus, clonidine decreases heart rate in dose dependent manner when given through epidural.
Fall in mean arterial blood pressure was observed after 45 minutes of epidural injection with maximum fall (21% in Group I and 19% in Group II) seen at 1 hour. The mean arterial blood pressure remained low till 2 hours in both the group. The maximum fall in the blood pressure within 1 hour can be explained by the systemic effect of clonidine. Also, the difference between the mean systolic blood pressure at 1 hour & 2 hour between the two groups was statistically significant (p<0.05), the mean arterial blood pressure being significantly lower in Group I as compared to Group II. No significant difference was observed in other reading between the two groups during rest of the time in study. None of the patients required treatment for hypotension.
Sedation score of 2 and 3 by Ramsay sedation scale and the sedation scores between the two groups were comparable with no statistically significant difference observed. The sedation lasted for 5-6 hours in both the groups. During this time the patients were easily aroused but asleep when not disturbed. Eisanach JC et al found that sedation following epidural clonidine was variable, not clearly dose-dependent, and lasted 1-3 hours. Observed that in clonidine 4μg/ml group, the degree of sedation was more severe and longer lasting than with lower concentration of clonidine, which necessitated careful monitoring of the patient.
We observed that there was no significant decrease in respiratory rate in both the groups (P> 0.05).
It is concluded from the present study that administration of clonidine given in epidural catheter is an effective and feasible technique for postoperative analgesia. Clonidine significantly leads to rapid onset of analgesia and prolongs the duration of postoperative analgesia and reduces postoperative analgesic consumption with initial bolus dose 150μg as compare to 100μg. Bradycardia which was noted in a few patients of 150μg group was easily treatable. Though the epidural clonidine leaves the patient calm, comfortable and minimally sedated, though easily arousable post operatively, initial bolus dose of 150 μg gives better analgesia and VAS score.