e-ISSN: 2320-7949 and p-ISSN: 2322-0090
e-ISSN: 2320-7949 and p-ISSN: 2322-0090
Department of Pedodontics, KVG Dental College and Hospital, Sullia, Karnataka, India.
Received:16 February 2014 Revised: 03/03/2014 Accepted: 13 March 2014
Visit for more related articles at Research & Reviews: Journal of Dental Sciences
Child visit to the dentist’s office can elicit fear and anxiety which can cause chaos to both the dentist and the child patient and, which in turn subvert the delivery of quality dental care, thus posing a challenge to oral health care practitioners worldwide. As pedodontists, our motto is to strive to relieve pain and suffering, and pledge to do no harm. Anxiety if not handled with tender love and care can be very devastating which has led to exploring new frontiers in behavior management. Behavior management with aversive methods using forced restraints, is no longer acceptable and may compound the hospital— and needle—phobia throughout life. Non pharmacological behavior management procedures like effective communication, distraction techniques, play therapy, modeling and adequate analgesia coupled with TLC may be sufficient to produce a cooperative, relaxed child. Assuming that the aforementioned non pharmacological behavior management techniques have failed, alternative pharmacological dental sedation methods is usually sought, in spite of moderate sedation with nitrous oxide being the safest mode of sedation, sedation with IV or IM ketamine remains one of the most used sedation technique popularly known as angel dust because of the unique magical experience of both the patient and the anesthesiologist using it. Bearing in mind that the perks of ketamine dissociative sedation are not free off its risks, the purpose of this article is to give the readers, an in depth knowledge of this agent. To deliberate; is ketamine sedation the answer for the inconsolable anxious child requiring a painful procedure in the pediatric dental department?
Fear is a primitive response developed in an individual; to protect him from harm and self-destruction; however fear should be channelized to only the harmful situation. Ironically, the child is not mature enough to differentiate the dental office from other fear producing stimuli, resulting in devastating manifestation of fear and anxiety especially when they perceive a decreasing modicum of control over the dental situation [1]. In fact, much dental fear is a manifestation of a simple lack of control and the actual physical discomfort is of secondary importance [2]. As the general protocol, at least one or two attempts are made using all available conventional behavior management techniques before the decision is made to utilize pharmacological behavior management protocol [3,4]. Pedodontists are trained with an array of psychological and non-pharmacological techniques of managing a child with dental fear and anxiety but some unmanageable children may need the use of pharmacological management, conscious sedation and general anesthesia and pharmacological-sedative treatment modalities may be absolutely vital for the compassionate and effective treatment of dental phobic and special needs patients.
Sedation dentistry is indicated, is recommended and is the treatment of choice when the dental disease is interfering with, or has the potential to interfere with, the health and general wellbeing of the patient, and the patient does not have the capacity to tolerate reasonable, routine, and customary dental care in the state of consciousness. The paradox is the trend changing more towards pharmacological dental sedation strategies. It is a need of the hour and especially important is to weigh the risks of not providing dental care for a child with dental disease against the inherent risks and complications of utilizing sedation dentistry.
Ketamine is one of the most commonly used anesthetic agents available, with potent analgesic, hypnotic and amnesic effects [5]. When used correctly, it is a very versatile drug as complete analgesia permits performance of extremely painful procedures and amnesia is very helpful in helping the child forget the after effects of the dental procedures.
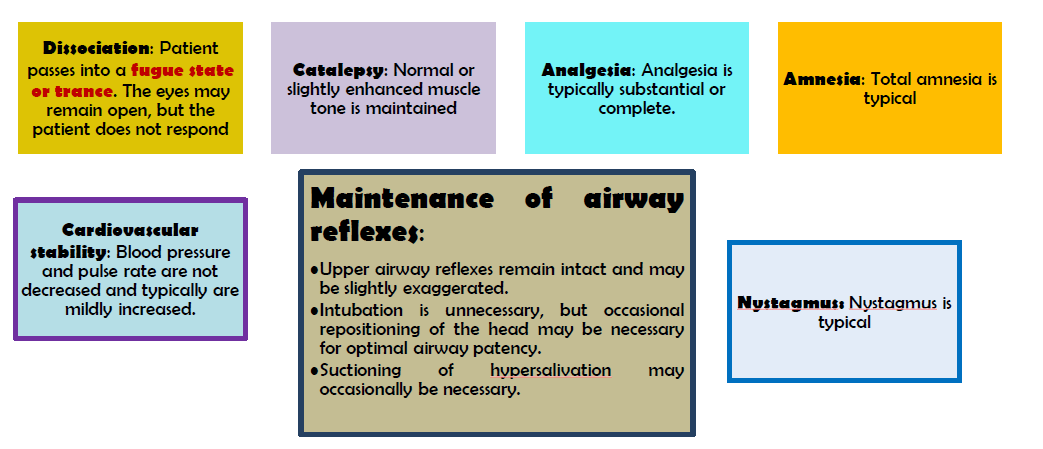
Ketamine is a phencyclidine derivative described in 1965, and first used in clinical practice in the 1970s. According to American College of Emergency Physician, ketamine sedation/dissociative sedation is defined as A trancelike cataleptic state characterized by profound analgesia and amnesia, with retention of protective airway reflexes, spontaneous respirations, and cardiopulmonary stability [6,7].
Ketamine may be administered by a variety of routes as it is both water and lipid soluble. Intravenous, intramuscular, oral, rectal, subcutaneous, epidural and transnasal routes have all been used [8].
Rather than displaying the dose-response continuum observed with all other procedural sedation and analgesia agents, ketamine dissociation appears at a dosing threshold of approximately 1.0 to 1.5 mg/kg intravenously (IV) or 3 to 4 mg/kg intramuscularly (IM). In smaller doses, ketamine exhibits analgesia and disorientation [9]. Once the dissociative threshold is reached, administration of additional ketamine does not enhance or deepen sedation, as would be the case with opioids, sedative-hypnotics, or inhalational agents. It should be noted that ketamine is not administered until the physician is ready to begin the procedure because onset of dissociation typically occurs rapidly [10,11].
As with all sedation regimens, stringent standard presedation assessment must be performed and documented with specific emphasis on prior hospitalizations, drug allergies, cardio – respiratory status, ASA classification of the patient and NPO. Educate accompanying family about the unique characteristics of the dissociative state if they will be present during the procedure or recovery. Frame the dissociative encounter as a positive experience. Consider encouraging older children to plan specific, pleasant dream topics in advance of sedation (believed to decrease unpleasant recovery reactions). Emphasize, especially to school-aged children and teenagers, that ketamine delivers sufficient analgesia, so there will be no pain [12].
• Prophylactic anticholinergics are no longer recommended.
• Prophylactic benzodiazepines are no longer recommended for children; however, they should be available to treat rare, unpleasant recovery reactions, should they occur. Prophylactic midazolam 0.03 mg/kg IV may be considered for adults.
• Prophylactic ondansetron can slightly reduce the rate of vomiting (number needed to benefit 9 or more).
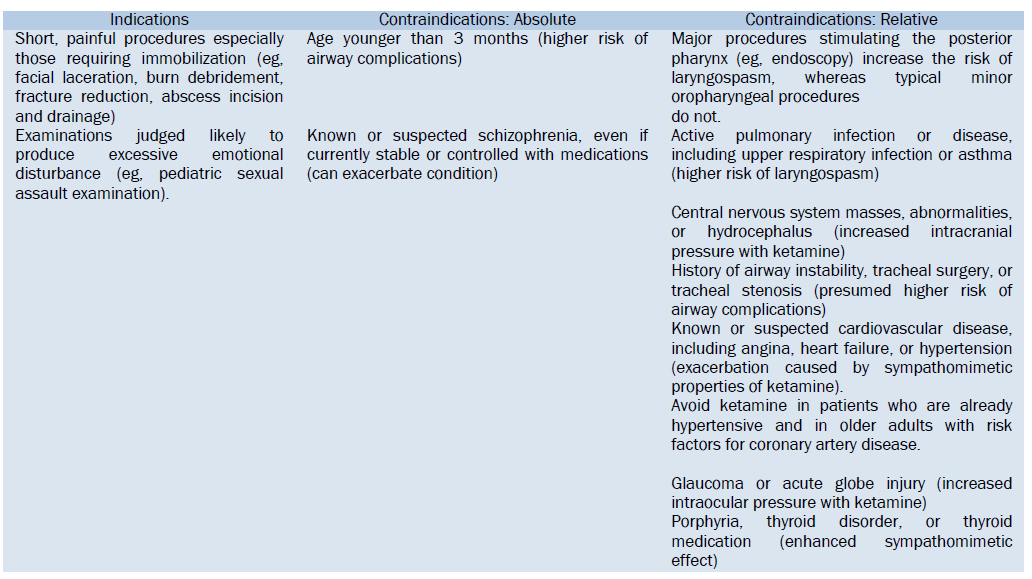
During ketamine anesthesia the airway is usually well maintained with some preservation of pharyngeal and laryngeal reflexes [7,9,11]. Extreme caution is advised thence during procedures that trickle the posterior oropharynx like intubation and extubation and the care should be taken to prevent aspiration nevertheless. Ketamine however, in addition to the general complications of sedation dentistry like cardio – respiratory depression, bronchospasm, apnoea, tracheal collapse, edema or infection of larynx/trachea aspiration of gastrointestinal contents and vocal cord paralysis, has had a reputation for increased rates of laryngeal spasm. Many of these reports may be due to partial airway obstruction with blood, saliva or emesis, which is very common with ketamine and usually responds to simple airway manoeuvres. Pooled data have shown that laryngospasm with ketamine sufficient to require intubation occurred in only 0.02% of cases compared with 1.75% of cases performed with agents other than ketamine [17]. Ketamine is to be infused slowly because rapid intravenous injection causes transient apnoea occasionally; this is easily managed with a brief period of bag-mask ventilation. These apnoeas are thought to be due to a reduced responsiveness to carbon dioxide with the high peak concentrations of ketamine seen after rapid injection. There is evidence that this apnoea may be seen more frequently in neonates [18].
Ketamine acts as a bronchodilator probably by two different mechanisms – firstly, via a central effect inducing catecholamine release, thereby stimulating b2 adrenergic receptors, resulting in bronchodilation, and secondly, via inhibition of vagal pathways to produce an anticholinergic effect acting directly on bronchial smooth muscle [19]. Whilst there is positive randomised controlled trial evidence for the use of ketamine for moderate to severe asthma in children [20], this has not been demonstrated in adults, although there are many case reports and small series attesting to its effectiveness.
Ketamine produces an increase in blood pressure, stroke volume and heart rate whilst maintaining systemic vascular resistance. These effects usually reach a maximum about 2 min after injection and settle over 15–20 min. There is a wide variation in individual response, and occasionally there can be a large rise in blood pressure, unrelated to a pre-operative history of hypertension [21]. It is thought that these adrenergic responses are mediated centrally and the use of centrally depressant premedication such as benzodiazepines can blunt this effect. Whilst ketamine has been shown to increase coronary blood flow, the benefit of this is probably negated by its effect on increased myocardial oxygen demand [22].
Ketamine produces dissociative anaesthesia (detached from surroundings). This is characterized by the patient often having their eyes open and making reflex movements during anesthesia and surgery. Frequent repeated sedation or anesthesia with ketamine such as that often experienced by burns patients can lead to tolerance with increasingly large doses being required. This tolerance generally lasts for 3 days. In recovery the patient may become agitated – this is due to hallucinations following ketamine anesthesia. The reported frequency of these hallucinations varies widely from 5 to 30%. The incidence of hallucinations is lowest in children. Increased incidence is associated with female sex, large doses of ketamine and rapid intravenous boluses. Hallucinations can be reduced by premedication with benzodiazepines (usually diazepam 0.15 mg/kg) orally 1 h pre-operatively or 0.1 mg.kg)1 intravenously on induction) or, alternatively, promethazine, which has the added advantage of an anti-emetic effect. Promethazine may be given as an oral premedication (age 2–5 years 15–20 mg per os (p.o.), 5–10 years 20–25 mg p.o.) or intravenously at induction (25–50 mg intravenously in the adult). It is not recommended for use in children less than 2 years old due to the risk of severe respiratory depression. Other benzodiazepines that have been used successfully include midazolam (0.05– 0.1 mg/kg) intravenously) and lorazepam (2–4 mg intravenously in the adult). Small doses of propofol and thiopental have also both been used successfully to attenuate hallucinations [7].
Ketamine has been shown to have both pro- [25] and anti-convulsant [26] effects. Due to the uncertainty of its effect in any one patient it is probably best avoided in epilepsy. In patients with schizophrenia, ketamine may reactivate no long-term psychotic reactions from the use of ketamine. Ketamine should be avoided in patients with a history of psychosis.
Ketamine increases salivation, which can lead to airway problems such as laryngeal spasm or obstruction. It may also make the taping of tracheal tubes more difficult. To reduce salivation, atropine is usually given either as premedication (20 mg/kg) intramuscularly to maximum 0.5 mg) 30 min pre-operatively or at the time of induction intravenously (10–20micro g/kg to maximum 0.5 mg). Alternatively, glycopyrrolate may be used (0.01 mg/kg) to maximum 0.2 mg intravenously).
Ketamine has a greater propensity to cause nausea and vomiting compared to thiopental or propofol; however, due to its opioid-sparing effects in the peri-operative period, the overall incidence of postoperative nausea and vomiting is reduced [7].
Ketamine increases skeletal muscle tone. This is most noticeable after the initial intravenous bolus and gradually decreases. It may be improved by administration of benzodiazepines [7].
Induction with ketamine produces a small rise in intraocular pressure which is still sustained 15 min into anaesthesia. In human studies this rise has not been found to be clinically significant and is smaller than that produced by laryngoscopy. The putative mechanism for this rise is increased tone of the extra-ocular muscles coupled with increased blood flow due to the increased cardiac output and a rise in arterial pCO2 seen with ketamine. Balanced anaesthesia with controlled ventilation helps to reduce these effects and in addition reduces the nystagmus otherwise commonly seen with ketamine anaesthesia.
In the case of the open eye or glaucoma, ketamine is still best avoided in favour of agents that produce no rise in intra-ocular pressure and that can attenuate the response to intubation [7].
Ketamine has been reported to produce hypertension and supraventricular tachycardia in patients who are hyperthyroid or receiving thyroxine. For this reason it is recommended to avoid ketamine in these patients [7].
Ketamine produces a serum rise in porphyric markers but no clinical evidence of porphyria. If an alternative, nonporphyria- inducing agent to ketamine is available, it should be used [7].
Ketamine causes an elevation in intracranial pressure by producing cerebral vasodilation and increased perfusion pressure. Ketamine is therefore relatively contraindicated in patients with serious head trauma, hydrocephalus, and intracranial lesions, since medullary compression may cause apnea. Finally, ataxia and dizziness may persist for up to 4 hr after ketamine administration. Therefore, rapid independent ambulation is not recommended following the use of ketamine [7].
The ketamine literature in children is robust enough to support fairly reliable estimates of the frequency of specific adverse events, as detailed further in this section. This is not yet possible in adults; however, their experience can be predicted to roughly parallel that of children unless contrary evidence is cited below.
In the large meta-analysis, airway or respiratory complications were observed in 3.9% of children overall, including transient laryngospasm in 0.3% and transient apnea in 0.8%. Misalignment of the airway may occur at any time during dissociative sedation, and stridor or hypoxemia should be initially treated with airway repositioning. The large meta-analysis showed no association of laryngospasm with any clinical factors, except a slightly greater risk with unusually high IV doses. A case control analysis found no association of age, dose, oropharyngeal procedure, underlying physical illness, route, or coadministered anticholinergics associated laryngospasm is rare (0.3% in a large meta-analysis), and the evidence supports it as largely idiosyncratic. However, clinicians administering ketamine must be prepared to rapidly identify and manage this adverse event. Although some patients may require bag-valve-mask ventilation, tracheal intubation because of ketamine-associated laryngospasm is rare [27,28].
Respiratory depression and apnea are unusual with ketamine and are transient when they do occur. Although most commonly associated with rapid IV administration, they can rarely occur with the IM route. When respiratory depression is noticed, it is invariably at the time of peak central nervous system levels (ie, 1 to 2 minutes after IV administration or 4 to 5 minutes after IM administration) [29].
Early adolescence is the peak age for vomiting, with lesser risk in younger and older children. The literature supports it as being more frequent with the IM route compared with IV and supports no evidence of a dose relationship within the usual range of clinically administered doses. When emesis occurs, it is typically late during the recovery phase when the patient is alert and can clear the airway without assistance. Vomiting does occur in some patients after discharge, including some who do not vomit in the ED. The incidence of vomiting in adults can be expected to be 5% to 15% [30].
The first and most practical of non-pharmacological behavior management techniques consists of good general communication practices aimed at calming all dental patients. Its defining qualities include an appropriately slow pace, careful selection of specific positive language and the avoidance of specific negative words, a calming tone of voice, and alignment of the entire office staff. It is essential that fearful patients are told the truth and that any promises made to them, casual or formal in nature, are kept. Psychological methods, insofar as they can be shown to be empirically effective, must be seen as an essential skill of the ethical dental practitioner1. Assuming that the non-pharmacological behavior management techniques have failed, alternative pharmacological dental sedation methods is usually sought, in spite of moderate sedation with nitrous oxide being the safest mode of sedation, sedation with IV or IM ketamine remains one of the most popularly used sedation antidote in the era of pediatric dental sedation.