e-ISSN: 2320-7949 and p-ISSN: 2322-0090
e-ISSN: 2320-7949 and p-ISSN: 2322-0090
1Department of Prosthodontics, Rama Dental College, Kanpur, India.
2Department of Prosthodontics, Dental College, Azamgadh, India.
3Department of Prosthodontics, Rajasthan Dental College and Hospital, Jaipur, India.
Received: 03/04/2013 Revised: 17/04/2013 Accepted: 19/04/2013
Visit for more related articles at Research & Reviews: Journal of Dental Sciences
Osteo-Odonto-Keratoprosthesis (OOKP) or ‘Tooth-in-eye surgery’, the original technique was described by Benedetto Strampelli nearly fifty years ago, using the patient’s own tooth root and alveolar bone as vital support to an optical cylinder, for patients with the most severe type of corneal and ocular surface diseases, for whom other treatments would not be useful. The cornea is replaced by a polymethyl methacrylate (PMMA) optical cylinder glued to a biological support (haptic) made by human living tissue. Prof.Giancarlo Falcinelli has refined and improved this procedure, in a step wise manner. OOKP surgery requires multidisciplinary team approach. Possible complications of this procedure include ulceration of the implant buccal mucosa, ocular infection and secondary glaucoma. This review article describes the Osteo-Odonto-Keratoprosthesis (OOKP) indications, surgical procedures, advantages and limitations.
Osteo-Odonto-Keratoprosthesis (OOKP); Biological Skirt; Keratoprosthesis (KPro); Osteo-dental acrylic complex (ODA complex).
Corneal opacification is the second most common cause in the world for blindness affecting an estimated 10 million people, in which corneal blindness is far more prevalent, as a result of ocular surface disease leading to corneal neo-vascularisation and scarring. Benedetto Strampelli described the original technique of Osteo-Odonto-Keratoprosthesis (OOKP) nearly fifty years ago, using the patient’s own tooth root and alveolar bone as vital support to an optical cylinder[1].Falcinelli G modified this technique in a stepwise fashion[2-6].
A Keratoprosthesis is used to replace damaged cornea. The Osteo- Odonto -Keratoprosthesis (OOKP) also known as ‘tooth in eye surgery’ is an auto graft used for the treatment of severe corneal opacities not suitable for corneal transplantation. The cornea is replaced by a polymethyl methacrylate (PMMA) optical cylinder glued to a biological support (haptic) made by human living tissue. Currently available KPro devices range from the totally synthetic, such as the Boston KPro, to the totally biological tissue-engineered artificial cornea. The Osteo-odonto-Keratoprosthesis combines a synthetic optic with a biological haptic [7].
Indications for OOKP
• The corneal lesions resulted from Stevens-Johnson syndrome,
• Lyell syndrome,
• Trachomatous chronic conjunctivitis,
• Erythema multiforme,
• Vascular corneal surgeries,
• Trauma limited only to cornea,
• severe Pemphigoid and
• Chemical injuries [8].
Contra-Indications for OOKP
Patients who are suffering with Glaucoma, Patients under 17 years of age and patients with repeated graft rejections are contra-indications for OOKP surgery. Smoking and Betel nut chewing are contra indicated because smoking may cause graft vascularization problem and betel nut chewing will compromise tissue quality [8].
Advantages of OOKP
The OOKP is a true heterotopic auto graft made of living, long-lasting human tissue, which includes (1). The haptic is made of dentine, a hard tissue with a slow metabolic exchange, which may help to confer stability to the complex ODA lamina through a tight and long-lasting contact by means of acrylic resin with the PMMA optical cylinder and provide protection against cylinder extrusion and fistulization. This living material is the most suitable as a long-term support to the optical component of the KPro, with the lowest risks of extrusion and infection. (2). The properties of dentine as an avascular tissue in contact with both the corneal surface and the optical PMMA cylinder may prevent or limit the frequency of formation of retro prosthetic membranes. The tight, contact between the mucous epithelium and the components of the osteodental lamina (i.e., the dentoalveolar ligament, bone, and dentine, which generate an "epithelial seal" to the anterior chamber) prevents infection, leakage of the aqueous humor, infection, and tissue neovascular proliferation, which are mainly responsible for the formation of retro prosthetic membranes.(3).The living osteodental lamina may provide immune defense characteristics to the prosthesis, protecting against infections. Postoperative endophthalmitis associated with poor tooth conditions can be prevented before surgery [9].
Disadvantages of OOKP
It is a two-stage Surgery, requires lifelong follow-up, and aesthetic co-efficient is average [9].
Ideal Keratoprosthesis
The ideal device should be able to surpass the natural cornea by having an improved optical quality, with decreased aberrations and a specifiable power. It should have excellent biointegration, provide resistance against infection and last for lifetime of the patient. It should replicate some of the qualities of the cornea such as drug penetration and allowing intraocular pressure measurement.
The types of Keratoprosthesis currently available vary in design, especially regarding the support for the optical cylinder. Most models use a non-biological skirt that is often porous e.g. all PMMA, Dacron, expanded PTFE and Hydro gel. Keratoprosthesis with biological skirts were also developed, as they were thought to be closer related to the corneal tissue so that they would integrate better and be more compatible, such as the Strampelli’s OOKP using autologous tooth root and alveolar bone as a support for a PMMA optical cylinder.
OOKP surgery differs in several ways from other techniques like, multi-stage (usually two-stage) surgery is required, and there is surgery both in the mouth and in the eye. The OOKP could uniquely withstand a hostile dry keratinized ocular surface. Falcinelli devised stepwise modifications to the original Strampelli’s technique, which have led to improved visual results and retention of the device.
Surgical Procedure
OOKP surgery is usually carried out in only one eye. The other eye, if existing, should be kept as a ‘spare’ eye [7]. Cases are usually selected following assessment by a multidisciplinary team consisting of an ophthalmologist, maxillo-facial surgeon, radiologist and psychologist. This multidisciplinary input has an important bearing on the subsequent success of surgery. The surgical procedure used in patients consists of two fundamental stages separated by an average period of twelve weeks. The gap allows soft tissue to grow around the Osteo-Odonto lamina and for ocular surface reconstruction with buccal mucous membrane grafting to become vascularised. Buccal mucosa harvested from the inside of my cheek, was then stitched over the eye to be operated on, and stitched into place under the lids. It too would gain a blood supply over the next 2-3 months. Th buccal graft must be full thickness mucosa and of an area large enough to extend from medial to lateral canthi and from upper to lower lid fornices. This usually means harvesting a graft of 3 centimeters in diameter [10].
Stage 1
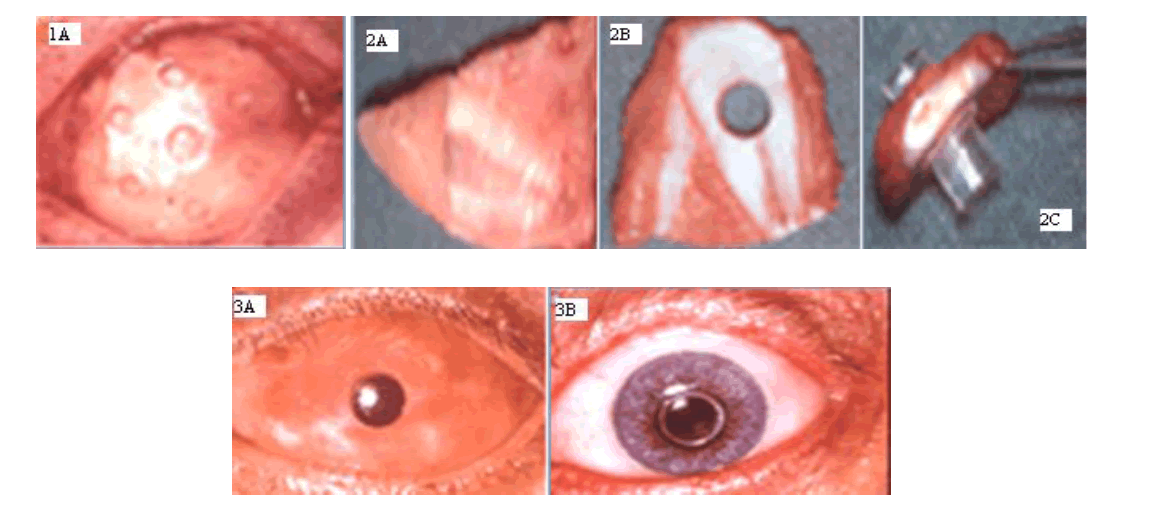
In the 1st Stage, a single rooted tooth (maxillary canine is the ideal tooth, because of its longest root, ideal tooth size and shape with the best surrounding alveolar bone) is harvested, to prepare an Osteo-Odonto lamina [Fig-2A]. The root and surrounding jaw bone is sliced and then removed by cutting across the bridging bone. The crown of the harvested tooth is used as a handle, whilst the attached
tooth root and surrounding bone is worked into a lamina with dentine on one side and bone on the other side, then pulp is removed. Periosteum is conserved and where possible glued back with fibrinogen adhesive. A hole is drilled through the dentine [Fig-2B] to accommodate a Poly Methyl Metha Acrylate (PMMA) optical cylinder, which is cemented in place [Fig-2C]. The crown portion of the tooth is removed prior to cementation of the optical cylinder. The resultant Osteo-Odonto lamina is placed into a sub-muscular pocket under orbicularis oculi, usually in the lower lid of the fellow eye, for a period of 2-4 months, in order to acquire a soft tissue covering. A buccal mucous membrane graft is used to cover the ocular surface [Fig-1]. It will be vascularized by the time of Stage 2 surgery and will subsequently provide the blood supply to the bone part of the Osteo-Odonto lamina.
Stage 2
This is carried out two to four months after stage 1surgery and this gap allows soft tissue to grow around the Osteo-odonto lamina and for ocular surface reconstruction with buccal mucous membrane grafting to become vascularised. Stage 2 Starts with retrieval of the Osteo-odonto lamina from its sub-muscular pocket. After retrieval, the excess soft tissue is removed from the bone surface. On the dentine surface, no soft tissue is allowed to remain. Then the lamina is trimmed to place a Flieringa ring and is sutured in place. The buccal mucosal graft is reflected to allow access to the cornea. Intravenous mannitol has by then been administered to reduce the intra ocular pressure. The centre of the cornea is marked, and a small hole is trephine, the diameter of which corresponds to that of posterior part of the optical cylinder. Relieving incisions are made. The iris is then completely removed. The posterior part of the lamina is inserted through the central corneal hole and the lamina is sutured onto the cornea and sclera. The eye is re-inflated with filtered air. The Flieringa ring is then removed. The mucosal flap is replaced after cutting a hole to allow the protrusion of the anterior part of the optical cylinder. At the end of the procedure, the patient is kept in the supine position for 5 to 6 days until complete resorption of intravitreal air (verified by either ophthalmoscopy or echography). Postoperative medical treatment includes antibiotics, corticosteroids, and ocular hypotensive drugs (acetazolamide) administered systemically. Intraocular pressure is routinely controlled daily up to at least 10 days. One month after surgery, [Fig-3A &B] a cosmetic prosthesis placed over the external ocular surface [9,10,11].
The Osteo–Odonto–Keratoprosthesis (OOKP) although described over 50 years ago remains the Keratoprosthesis of choice for end-stage corneal blindness. It is particularly resilient to a hostile environment such as the dry keratinized eye. Patients are advised to stop smoking among other measures to maintain good oral hygiene, which additionally improves the chance of survival of the buccal mucous membrane graft [7].
Many studies are available on the success of the OOKP surgery. Liu C, et al reported excellent long term retention of 85% in 18 years [10]. According to Herold J and his colleagues 80% of patients achieved improvement of vision [11]. Liu C, Masahiko F, and Yoshikazu S, stated that Osteo-Odonto-Keratoprosthesis (OOKP) described by Strampelli, and modified by Falcinelli gives the best long-term results for visual acuity of 75% with 6/12 or better, and retention of 85% for up to 18 years [12]. Giancarlo Falcinelli et al described the long-term anatomical and functional outcome in 181 cases and the results indicated that modified OOKP surgery can provide favorable anatomical and functional results, which are stable in the long-term and retaining an intact OOKP was 85% [9]. Tay AB et al conducted a retrospective study on 21 patients to describe the oral procedures used in OOKP surgery which utilized an autologous tooth-bone complex to mount a poly-methylmethacrylate optical cylinder, as an artificial cornea, stabilized by an overlying autologous buccal mucosal graft. Complications included fracture of a tooth from its lingual bone necessitating the harvesting of a second tooth, oronasal perforation, exposure of adjacent roots, lower lip paresthesia and sub mucosal scar band formation in the buccal mucosal graft donor site[13] . Tan et al treated 29 cases to restore sight with OOKP surgery found excellent results without any instability problems or extrusion [14]. Hughes et al, reported vitreoretinal complications of the OOKP in a retrospective review of 35 patients, follow-up at a mean 57 months, revealed that 9 vitreoretinal complications in 8 patients (23%) were found [15]. Kumar RS et al did a Study, to report diagnostic modalities and treatment options for glaucoma in 15 eyes that underwent OOKP surgery and they concluded that visual field testing and optic disc assessment with optic disc photographs seem to be effective methods to monitor eyes with OOKP for glaucoma, and treatment strategies include oral medication (acetazolamide 500 mg twice a day) to lower intraocular pressure and cyclophoto coagulation [16]. Skelton VA et al explained the surgical process of Osteo-Odonto-Keratoprosthesis surgery with reference to anaesthetic experiences from 9 cases, patients with bilateral corneal blindness in whom corneal transplantation has either been unsuccessful or inappropriate may be considered for Osteo-Odonto-Keratoprosthesis surgery [17].
The Role of Dental Surgeon
The Dental Surgeon will do the Oral assessment of the patient who is undergoing for OOKP, for both the buccal mucosal graft donor site and a selection of an appropriate tooth to form a dentine/bone lamina. The assessment aims to select a healthy tooth (root) with the best shape and size with good covering of alveolar bone. The surrounding anatomy is assessed to avoid possible complications and to reduce the cosmetic defect to a minimum. The overall oral health with particular reference to oral hygiene and periodontal bone loss must be assessed. Clinical assessment of bone loss can be useful but radiographs are essential. The mainstay radiological views are ortho pantomograms (OPG), and intra-oral periapical radiographs (IOPAs).These views will give enough information. CT scan can be useful to get more details. One month after OOKP surgery, a cosmetic prosthesis which covers the external ocular surface is usually applied and replacement of missing tooth may be made by means of placing an implant support prosthesis or use any other prosthesis as the patient wishes.
Complications
Possible complications of this procedure include ulceration of the implant buccal mucosa, ocular infection, secondary glaucoma, extrusion, retinal detachment and retroprosthetic membrane formation [18,19].
Follow-Up Visits
Follow-up is life-long in order to detect and treat complications, which include oral, oculoplastic, glaucoma, vireo-retinal complications and extrusion of the device. At weekly intervals for one month, then monthly for three months, then every two months for six months, then every four months for stability of the prosthesis and intraocular pressure measurements .Once it became stable follow-up can be at longer interval [9,10].
Emerging Devices
Research groups around the world have recently tried several new approaches, with the aim of reaching an ideal KPro. The Supra Descemetic Synthetic Cornea (SDSC) is one of these devices, developed by Parel, Lacombeand Alfonso in 1990. Another promising project funded by the European Union (EU-Project CORNEA No. 017905), researchers are evaluating a newly designed hydrophobic implant made of a single material with modified surface coatings. Initial results showed good biointegration of the fibronectin-coated haptic, cell free transparency of the optic and suitability for fibronectin-coated haptic, cell free transparency of the optic and suitability for epicorneal fixation. 51 Initial human trials were due to start in Germany in June 2008. At Stanford University (CA, USA), researchers used a mechanically enhanced hydrogel material called Duoptix to develop a new ‘core and skirt ’KPro. Recent advances in tissue engineering have now made it possible to produce natural corneal substitutes from recombinant human collagen. Results of in vivo animal studies show good integration, with regeneration of corneal cells, including nerves and tear film production [7].
The OOKP is considered the only device capable of offering long-term visual rehabilitation in patients with end-stage ocular surface disease with severe tear deficiency (with or without lid defects). The surgical technique involves the removal of the canine tooth for the preparation of the Osteo-dental-acrylic lamina complex. Modern OOKP surgery is the only hope for restoring sight in the long term for desperate cases of corneal blindness not amenable to conventional corneal surgery. OOKP surgery is complex and requires meticulous care at each step to ensure the overall success rate. Oral structures have to be sacrificed.