e-ISSN: 2320-7949 and p-ISSN: 2322-0090
e-ISSN: 2320-7949 and p-ISSN: 2322-0090
Nikhila Nemmarugommula1, Arun A2, and Mythri H3*
1Kamineni Institute of Dental Sciences, Narketpelly, Nalgonda, Andra Pradesh, India.
2Dept. of Conservative Dentistry, Sree Siddhartha Dental College and Hospital, Tumkur, Karnataka, India.
3Dept. of Public Health Dentistry, Sree Siddhartha Dental College and Hospital, Tumkur, Karnataka, India.
Received: 10/08/2013 Revised: 28/08/2013 Accepted: 15/09/2013
Visit for more related articles at Research & Reviews: Journal of Dental Sciences
Caries activity tests have been well known in dentistry for the past few years. However, it is still difficult to determine which method is the best to estimate the possibility of caries occurrence in individuals. A good caries prediction test which can indicate its value in predicting the future occurrence of caries is required.
caries, organisms, saliva, streptococcus
Caries activity tests are based on the concept of a specific odontopathic infection, the principle causative organism being Streptococci mutans. Their predominance is attributed to its acidogenic and aciduric nature after a selective growth advantages over the other non-acid tolerant organisms [1].
It is difficult to identify caries susceptible children on the basis of a visual and tactile oral examination. Many bacteriological caries activity tests have been developed to avert this difficulty. They are classified into two types: count method and evaluation of bacterial virulence. Borgström and colleagues reported that the most common method used to identify caries-susceptible people is estimating the number of cariogenic bacteria such as lactobacilli and mutans streptococci in saliva or plaque samples taken from the patient [2].
Many studies on caries activity are aimed at finding relevant micro organisms. But to date, the ideal method to evaluate in terms of sensitivity, specialization and reliability has not been found. However, in routine clinical practice these caries activity tests require specially prepared culture media and laboratory facilities for incubation and expensive kits to perform them [3].
Unfortunately, many of these caries activity tests require extensive work up time and additional equipment. Simple, inexpensive techniques, which do not demand, sophisticated skills or consume much time are required for the caries activity tests and the status they deserve in the routine clinical practice and epidemiological screening programs [4].
Stolpe J R classified it under 3 headings;
1. Tests concerned with chemical properties of Saliva
2. Tests concerned with bacterial constituents of Saliva
3. Tests which measure certain changes in chemical properties produced by bacterial metabolism.
Uses [5]
• Establish a baseline level of cariogenic pathogens as a basis for future evaluation and counselling.
• Ensure a low level caries activity before starting any extensive procedures.
• To modify the patient behaviour as a part of counselling to restrict sucrose intake.
Advantages
• Identification of high risk population for dental caries and to institute effective preventive measures.
• In depth analysis of caries progression by researchers and to develop better control measures.
• Decreases the caries susceptibility at individual level.
Criteria for an ideal Caries activity test
• Should be simple & inexpensive
• Should be valid
• Should be reproducible
• Should be sensitive
• Should be measurable
• Should be non– invasive and applicable to any clinical setting
Definitions
Caries activity: increment of active lesions over a stated period of time.
Caries susceptibility: susceptibility (or resistence) of a tooth to a caries producing environment.
A. Tests which measure caries activity
• Lactobacillus colony count test
• Streptococcus mutans level in saliva
• S. Mutans screening tests
– Plaque-tooth pick method
– Saliva/tongue blade method
– S. Mutans adherence method
– S. Mutans dip-slide method
– S.mutans replicate technique
• Alban test
• Dewar test
• Swab test
• Salivary buffer capacity test
B. Tests which measure caries susceptibility
• Snyder’s colorimetric test
• Enamel solubility test
• Dewar test
• Fosdick calcium dissolution test
• Salivary reductase test
Others
• Ora test
Lactobacillus Colony Count Test
Principle involved: Estimation of the number of acidogenic and aciduric bacteria in the patient saliva by counting the number of colonies appearing on Tomato peptone agar plates (pH 5.0) after inoculation with a sample of saliva.
Procedure
• Immediately after arising, the patient chews a small piece of paraffin.
• The saliva that accumulates in the following 3-minute period is collected in a sterile container, and shaken well.
• The saliva sample is diluted to 1:10 dilution by sterile saline solution, and then 1:100 dilutions.
• 0.4 ml of each dilution is spread on the surface of an agar plate containing 20 ml of cooled liquefied agar (Rogosa’s SL agar plates, better then Tomato Peptone agar).
• Incubation at 37°C for 3-4 days.
• Counting of colonies using colony counter equipped with bright light and a large magnifying glass.
• The number of lactobacilli per mm saliva is calculated by multiplying the number of colonies on the plate by the dilution factor.
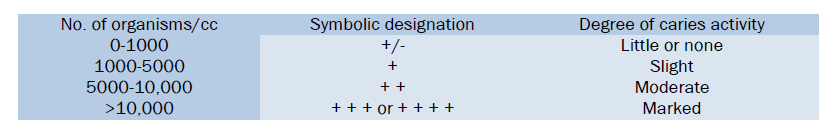
Interpretation:
Advantages
• Useful for monitoring the effectiveness of restorative dentistry.
• Simple to carry out.
• Useful as a screening test for caries activity in large groups.
Disadvantages
• Inaccurate for predicting the onset of caries.
• Does not completely exclude the growth of other aciduric organisms.
• Counts involving single individuals are not as reliable.
• Takes few minutes to do the test, but the results take several days.
• Counting is a tedious procedure.
Streptococcus Mutans Level in Saliva
Principle involved: Measures the number of S.mutans colony forming units per unit volume of saliva and plaque samples from discrete sites, such as occlusal fissures and proximal areas.
Incubation is done on Mitis Salivarius Agar(MSA), selective streptococcal medium with addition of high concentration of sucrose(20%), and 0.2 U Bacitracin (MSB), suppress the growth of most non-S.mutans colonies.
Procedure
• Sample collection by the use of tongue blades (wooden spatulas).
• Tongue blades then pressed against MSB Agar.
• Incubation at 37°C for 48 hours at 95:5 % CO2 gas mixture.
Interpretation: Levels of Streptococcus mutans > 105/ml of saliva is unacceptable.
Advantage: Useful in caries management as S.mutans are main causative agents.
Disadvantages
• Difficulty of distinguishing between a carrier state and cariogenic infection.
• S.mutans may constitute less than 1 % of total flora of plaque.
• S.mutans tends to be located at specific site only.
Streptococcus Mutans Screening Test
Plaque / tooth pick method:
Principle involved
Simple screening of dilutes plaque sample streaked on a selective culture media.
“Semi quantitative screening of dental plaque for S.mutans”
Equipments
Sterile tooth picks.
Sterile ringer’s solution (5ml).
Platinum Loop.
Mitis Salivarius Agar plates (MSA) containing sulphadimetine.
Procedure
• Plaque samples are collected from the gingival thirds of buccal tooth surfaces one from each quadrant and placed in Ringer's solution.
• The sample is shaken until homogenized.
• The plaque suspension is stretched across MSA plates.
• Aerobic incubation at 37°C for 72 hours.
• Cultures are examined and total colonies in 10 fields are recorded.
Saliva / Tongue Blade Method
Principle involved: Estimation of the number of S.mutans in paraffin-stimulated saliva when cultured in Mutans Salivarius Bacitracin (MSB) agar.
Equipments
Paraffin wax.
Sterile Tongue Blades.
Disposable Petri Dish containing MSB agar.
Procedure
• The subjects chew a piece of paraffin wax for one min to displace plaque microorganisms, to increase their proportion in saliva.
• Sterile tongue blades are rotated in the mouth 10 times so that both the sides are thoroughly inoculated with the subject’s flora.
• Tongue blades are then pressed into MSB agar.
• Incubation is done at 37°C.
• Numbers of colonies are counted.
Advantages
• Simple, practical method for field studies as there is no requirement of transport media/dilution.
• Suitable for use in the studies involving school children.
Dip-Slide (Dentocult-Sm) Method for S.Mutans Count
Principle involved: Estimation of Streptococcus mutans levels in saliva.
Procedure
• Undiluted paraffin- stimulated saliva is poured on a special plastic slide, coated with MSA(Mitis Salivarius Agar) containing 20% sucrose. The agar surface is thoroughly moistened and excess saliva is allowed to drain off.
• Two discs containing 5 mg of bacitracin are placed on the agar 20 mm apart.
• The slide is tightly screwed into a cover tube and incubated at 37°c for 48 hours in a sealed candle jar.
Interpretation
Score 1 =Low: The colonies are discrete and could be readily counted at 15X magnification with the total count of CFU inside the inhibitions zones less than 200.
Score 2 =Medium: The colonies are discrete and the number in the zone of inhibition is more than 200 and 32X magnification.
Score 3 = High: The colonies are tiny and almost completely or totally cover the inhibition zone with the number of colonies uncontrollable even with 32X magnification.
The Swab Test
Principle involved: Same as Snyder’s test.
Procedure:
• The oral flora is sampled by swabbing the buccal surfaces of teeth with a cotton applicator, which is subsequently incubated in the medium.
• The change in the pH following 48 hour incubation is read on a pH meter or colour change is read by the use of a colour comparator.
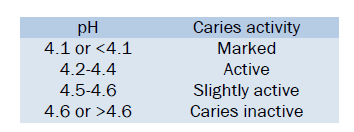
Interpretation:
Advantage: Useful in predicting caries increments or changes, particularly in children, as no collection of saliva is required.
Salivary Buffer Capacity Test
Principle involved: Buffer capacity can be Quantities using either a pH meter or colour indicators.
This test measures the number of milliliters of acid required to lower the pH of saliva through an arbitrary pH interval (6 to 7) or the amount of acid or base necessary to bring color indicators to their end point.
Equipments
Titration equipment
0.05 N lactic acid
0.05 N base, paraffin
Sterile glass jars containing a small amount of oil.
Procedure
• 10 ml of stimulated saliva is collected under oil at least I hour after eating.
• 5 ml of this is measured into a beaker.
• After correcting the pH meter to room temperature, the pH of saliva is adjusted to 7.0 by addition of lactic acid or base.
• Lactic acid is then added to the sample until a pH of 6.0 is reached.
• The number of ml of lactic acid needed to reduce pH from 7.0 to 6.0 is a measure of buffer capacity. (can be converted to milliequivalents per liter)
Interpretation
“Inverse relationship between buffering capacity of saliva and caries activity”.
The saliva of individuals whose mouths contain a considerable number of carious lesions frequently has a lower acid-buffering capacity than the saliva of those who are relatively caries free.
Advantage: Simple to carry out.
Disadvantage: Doesn’t correlate adequately with caries activity.
Calorimetric Snyder Test [9]
Principle involved: Measures the ability of salivary microorganisms to form organic acid from a carbohydrate medium. The medium contains an indicator dye “Bromocresol green”, changes colour from green to yellow when pH changes from 5.4 to 3.8. Indirectly measures the number of both aciduric and acidogenic organisms in saliva.
Procedure:
• 0.2ml stimulated saliva collected by chewing paraffin before breakfast is thoroughly mixed with 10 ml melted agar containing medium in a test tube (cooled to 50°C).
• Allowed to solidify and then incubated at 37°C.
• Amount of acid produced by acidogenic organisms is detected by changes in pH indicator, and is compared to an uninoculated control tube after 24, 48, and 72 hours.
• The rate of colour, change from green to yellow is indicative of the degree of caries activity.
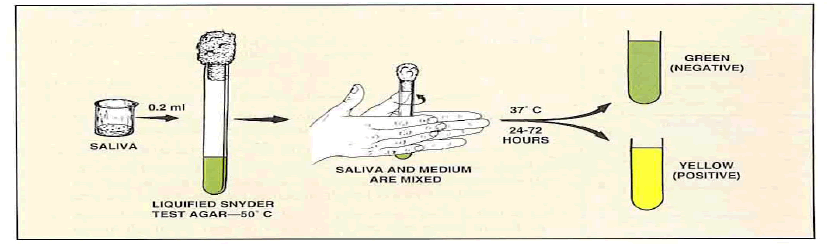
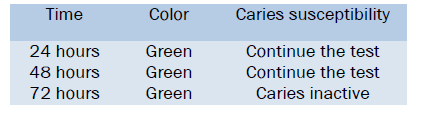
Interpretation
If the colour is yellow-
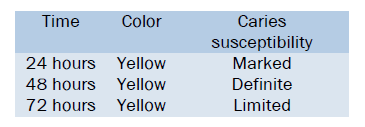
If the colour is green-
Advantages
• Relatively simple to carry out.
• Tests are of value in assessing the cariogenic challenge.
• Only one tube and no serial dilutions are required.
Disadvantages
• Time consuming.
• Sometimes the colour changes are not so clear.
Albans Test
It is a simplified substitute for the Snyder test.
Principle involved: Same as Snyder test.
Procedure: To prepare the Alban test medium:
Materials required
• Snyder test agar
• A small scale, to measure 60 grams.
• A 2 liter Pyrex glass, to melt the medium.
• A funnel, to dispense the medium into test tubes.
• 100, 16 mm test tubes with screw caps.
60 grams of Snyder test agar is placed in 1 liter of water and the suspension is brought to a boil over a low flame. When thoroughly melted, the agar is distributed about 5 ml per tube. These tubes should be autoclaved for 15 min. Then cooled and stored in a refrigerator.
Steps
• 2 tubes of Alban medium are taken from the refrigerator.
• The patient is asked to expectorate a small amount of saliva directly into the tubes.
• The tubes are labeled and incubated at 98.6°F (37°C) for up to 4 days.
• The tubes are observed daily for;
– Change of colour from bluish green (pH 5) to definite yellow (pH 4 or below)
– The depth in the medium to which the change has occurred.
• The daily results collected for a 4 day period recorded on the patient chart.
Interpretation
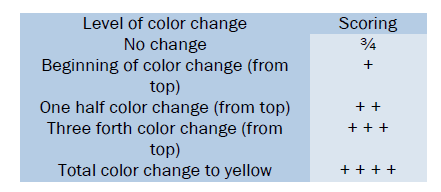
Inferences
• Readings negative for the entire incubation period are labeled- Negative.
• All other readings are labelled- Positive (+, + +, + + + or + + + +)
• Slower change or less colour change (compared to previous test) is labelled- Improved.
• Faster or more pronounced colour change (compared to previous test) is labelled- Worse.
• When consecutive readings are nearly identical, labelled as- No change.
Advantages
• Use of a somewhat softer medium that permits the diffusion of saliva and acids without the necessity of melting the medium.
• Use of a simpler sampling procedure in which the patient expectorates directly into tubes that contain the medium.
• Low cost.
• Diagnostic value even when negative results are obtained.
• Motivational value (ideal for education).
• Good for indicating caries inactivity.
Disadvantages
• More armamentaria required.
• Based on subjective evaluation of a colour change that is often not clear cut.
Salivary Reductase Test (Susceptibility Test)
Principle involved: Measures the activity of the reductase enzyme present in salivary bacteria, using a dye Diazo-resorcinol.
Procedure
• Saliva is collected in a plastic container.
• The sample is then mixed with the dye.
• The caries conduciveness is measured by color change, seen after 15 minutes. (A kit is availably under the trade name Treatex.)
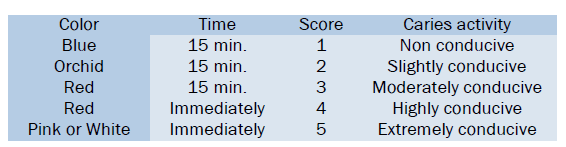
Interpretation: The evaluation is based on the color change
Advantages: Quick results, as no incubation period is required.
Disadvantage: Test results vary with time after food intake and after brushing.
Fosdick Calcium Dissolution Test
Principle involved: Measurement of amount of powdered enamel dissolved in 4 hours by acid formed, when the patient’s saliva is mixed with glucose and powdered enamel.
Procedure
• Saliva is stimulated by having the patient to chew gum or paraffin.
• 2.5 ml of saliva is collected.
• One part of this is used to analyze the calcium content.
• The remaining is taken into a 8 inch sterile test tube, in which 0.1 gm of powdered enamel is added.
• Test tube is sealed and shaken for 4 hours at body temperature.
• Then calcium content is analyzed.
• When paraffin is used to stimulate saliva, 5% glucose is added. (Chewing gum contains sugar).
Interpretation: Amount of calcium increases, as the caries activity increases.
Advantage: In the limited studies, correlation reported is good.
Disadvantages
• Requires complex equipment and trained personnel
• Expensive.
Dewar Test
Principle involved: Same as Fosdick Calcium Dissolution test.
Procedure: Same as Fosdick Calcium Dissolution test, difference is in Dewar test final pH after 4 hours is measured, instead of the amount of calcium dissolved.
This procedure is not commonly used, as it has not been adequately tested for clinical correlation.
Limitations of Current Caries Activity Tests
• Since caries activity tests measure a single parameter like acid production or colony count of bacterial species, none of these tests are highly reliable indicators of expected caries increments. It is better to use combination of tests to solve this problem.
• Most of the tests are time consuming.
• There is need to develop chair side tests.
Future Methods
A serious concern with the culturing methods of today is the time span from sampling until the results are available for the professionals and their patients. It is necessary to improve today’s methods to make them suitable for chair side use or for field condition.
New tests, measuring, for example, bacterial adhesion and bacterial binding saliva legends as genetically determining factors for caries, might be developed.
The growing interest in the microbiological aspects of dental caries has lead to the development of a variety of diagnostic procedures. A number of caries activity tests have been developed to help detect the presence of oral conditions associated with increased caries risk. For individual patients, currently no single caries activity test can be relied upon to predict caries with a high degree of confidence. Since, many of these tests rely on the samples of salivary bacteria. The reliability of such tests is limited, because the bacteria that are free-floating in the saliva may not necessarily represent the bacteria in plaque and these tests, also need extensive working time and expensive armamentarium [10].
Individual caries activity tests, despite their limitations can be useful adjuncts to the clinical practitioner, by guiding the clinician in making decisions concerning the need for control measures, the timing of recall appointments, the types of indicated restorative procedures, materials and the determination of the prognosis. The test results also can also be used to motivate patients and to determine patient compliance with treatment regimes. A simple, inexpensive technique, which does not demand sophisticated skills or consume less chair side time will help to give the caries activity tests the status they deserve in routine clinical practice [4].
Ora Test [4]
Oratest is based on the rate of oxygen depletion by micro organisms. Under aerobic conditions the bacterial enzyme, aerobic dehydrogenase transfers electrons or protons to oxygen. Once oxygen gets utilized by the aerobic organisms and an anaerobic environment is attained, methylene blue [redox indicator] acts as an electron acceptor and gets reduced to leucomethylene blue. The metabolic activity of the aerobic microorganism is reflected by the reduction of methylene blue to leucomethylene blue.
The test is based on rinsing the mouth with sterile milk which dislodges the micro-organisms and also produces a substrate for their further metabolism. The formation of leucomthylene blue can be easily observed because of the white colour of milk.
Caries activity tests have been well known in dentistry for the past few years [1-4]. However, it is still difficult to determine which method is the best to estimate the possibility of caries occurrence in individuals. A good caries prediction test which can indicate its value in predicting the future occurrence of caries is required.
The most important thing in the caries activity test on which attention should be paid lies in the active case selecting ability of the test, for interpreting the possible occurrence of caries in individuals in the attempt to improve the prevention program.
The value of a preventive attempt must indicate good effectiveness and efficiency, particularly for children with high caries risk. The theory and understanding of the caries process has developed quite rapidly, while the development of the formula to distinguish the caries prediction test is still relatively slow. It is important to establish the criteria in order to obtain a good caries prediction test, especially one that has a close relation to the dental caries prevention programs in the community [11].
A caries activity test facilitates the clinical management of patients as they determine the need and extent of personalized preventive measures. It serves as an index for the success of therapeutic measures and also help and to motivate and monitor the effectiveness of educational programs relating to dietary and oral hygiene procedures. It is of particular importance in identifying high - risk groups and individuals.