e-ISSN: 2320-7949 and p-ISSN: 2322-0090
e-ISSN: 2320-7949 and p-ISSN: 2322-0090
1Department of Orthodontics and Dentofacial Orthopedics; People‘s College of Dental Science and Research Centre; Bhopal; Madhya Pradesh, India.
2Department of Orthodontics and Dentofacial Orthopedics, Kothiwal Dental College and Research Centre; Muradabad; Uttar Pradesh, India.
Received: 23 January 2014 Revised: 05/02/2014 Accepted: 03 March 2014
Visit for more related articles at Research & Reviews: Journal of Dental Sciences
Seizure disorders are the most common serious chronic neurological condition. This review is intended to update the orthodontist regarding seizure disorders including etiology, medical and surgical management, impact on dental health, potential for altering orthodontic treatment planning and delivery, and guidelines for management of seizures in the orthodontic office. It is estimated that there are 55,00,000 persons with epilepsy in India, 20,00,000 in USA and 3,00,000 in UK. The majority of patients can be managed medically so that they remain free of seizures. Contemporary management may include medications, surgery, an implanted nerve-stimulation device, and/or a ketogenic diet. Considerations for the orthodontist planning treatment for a patient with a seizure disorder are specific details about seizure onset, frequency, and type, behavior during seizures, duration, triggers, recovery period, medical management, and compliance. Patients with epilepsy and a malocclusion should have a comprehensive orthodontic evaluation. Adverse side effects of Anti-Epileptic Drugs (AEDs) and past dental trauma should be researched by the orthodontist and reviewed as part of patient informed consent. The practitioner and staff should be prepared to recognize and respond appropriately when a patient has a seizure in the orthodontic office.
epilepsy, seizures, Orthodontic management, antiepileptic drugs
The majority of patients who are treated orthodontically are healthy young individuals. However, the last 20 years has seen a dramatic increase in the number of adult patients seeking orthodontic treatment, many of them suffering from chronic diseases. Advances in the management of many of these maladies have allowed these patients to pursue elective orthodontic procedures that only years ago would have been considered contraindicated. One such disease is epilepsy or seizure disorder. This review is intended to update the orthodontist regarding seizure disorders including etiology, medical and surgical management, and impact on dental health, potential for altering orthodontic treatment planning and delivery, and guidelines for management of seizures in the orthodontic office.
The word epilepsy is derived from the Greek word epilambanein meaning to take or to seize. A seizure is a sudden, involuntary, time-limited alteration in neurologic function resulting from abnormal electrical discharge of cerebral neurons. Seizures manifest as altered sensation, behavior, or consciousness [1]. The cumulative incidence of epilepsy from birth through age 20 years is about 1% and increases to 3% at age 75 [2]. It is estimated that there are 55,00,000 persons with epilepsy in India, 20,00,000 in USA and 3,00,000 in UK. Three to five per cent of the populations have a seizure sometime in their life and half to one per cent of the population have active epilepsy‘ [3]. About 30% occur in children. Children and elderly adults are the ones most often affected. There is a clear cause for epilepsy in only a minority of the cases. Typically, the known causes of seizure involve some injury to the brain. Some of the main causes of epilepsy include: low oxygen during birth, head injuries that occur during birth or from accidents during youth or adulthood, brain tumors, genetic conditions that result in brain injury, such as tuberous sclerosis, infections such as meningitis or encephalitis, stroke or any other type of damage to the brain, abnormal levels of substances such as sodium or blood sugar. Some patients have identified triggers that impact the number and severity of seizures. Examples of triggers are flashing lights, anxiety, illness, and hyperventilation. Factors reported to increase seizures include missed medication, sleep deprivation, stress, alcohol consumption, nonprescription medications, vitamin or mineral deficiencies, and parts of the menstrual cycle [4].
The seizure threshold is that level of excitement at which a neuron will discharge abnormally; it is determined, in part, by excitatory and inhibitory neurotransmitter influences on the cell. A seizure occurs when the balance between neuron excitation and inhibition is upset; when multiple cells fire simultaneously, a seizure will result. The brain has a margin of safety to prevent misfires; the size of that margin is determined genetically.
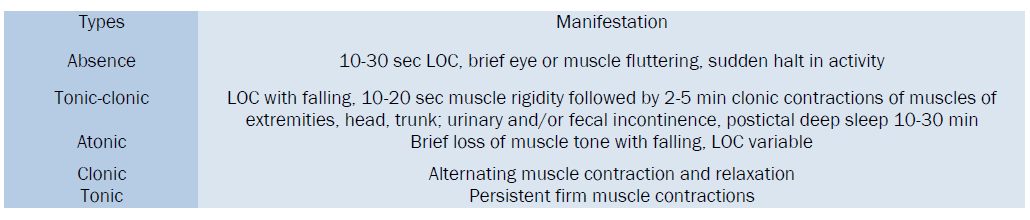
The initial classification was created in 1970, and then revised in 1981 [5]. The currently used classification of seizures is in Table 1. In addition to classifying seizures, in 1989 the ILAE (International League against Epilepsy) also classified the different epilepsies listed in Table 2. Figure 1. While many types of repetitive behavior may represent a neurological problem, a doctor needs to establish whether or not they are seizures.
All areas of the brain (the cortex) are involved in a generalized seizure. Sometimes these are referred to as grand mal seizures. Their incidence is estimated at 10 to 15 per 100,000 from infancy through age 65 years. The person experiencing such a seizure may cry out or make some sound, stiffen for several seconds to a minute and then have rhythmic movements of the arms and legs. Often the rhythmic movements slow before stopping. Eyes are generally open. The person may appear to not be breathing and actually turn blue. This may be followed by a period of deep, noisy breathes. The return to consciousness is gradual and the person may be confused for quite some time –minutes to hours. Loss of urine is common. The person will frequently be confused after a generalized seizure.
Only part of the brain is involved, so only part of the body is affected. The incidence of partial seizures is estimated at 20 per 100,000 from infancy through age 65 years. Depending on the part of the brain having abnormal electrical activity, symptoms may vary. If the part of the brain controlling movement of the hand is involved, then only the hand may show rhythmic or jerky movements. If other areas of the brain are involved, symptoms might include strange sensations like a full feeling in the stomach or small repetitive movements such as picking at one's clothes or smacking of the lips. Sometimes the person with a partial seizure appears dazed or confused. This may represent a complex partial seizure. The term complex is used by doctors to describe a person who is between being fully alert and unconscious.
These are most common in childhood. Impairment of consciousness is present with the person often staring blankly. Repetitive blinking or other small movements may be present. Typically, these seizures are brief, lasting only seconds. Some people may have many of these in a day.
The need for a diagnosis of epilepsy is usually precipitated by a first seizure. The physician must decide whether a seizure is in fact a real seizure or another condition such as fainting. There are three primary steps in the diagnosis of epilepsy: health history taking, neurological examination, and laboratory testing. A health history will include information about the facts surrounding the seizure. Sometimes the person has no memory of the event, therefore, eyewitness observation is very helpful. Family history, social history, and past medical history are also important in making a correct diagnosis A neurological examination will be done to identify areas of abnormal brain electrical activity, as well as assess the patient‘s motor and sensory skills, the functioning cranial nerves, hearing and speech, vision, coordination and balance, mental status, and changes in mood or behavior Depending on the heath history and examination findings, laboratory work may be ordered. This might include blood studies and special testing such as EEG, CT, MRI, PET, neurosonography, and lumbar puncture
Several disorders can often be mistaken for an epileptic seizure: hyperventilation, hypoglycemia, migraine, transient ischemic attacks, syncope, pseudoseizure, transient global amnesia, and sleep disorders. Of these, the most common conditions confused with epilepsy are syncope, pseudoseizure, and panic attacks.
Various first-generation antiepileptic drugs (AEDs) — phenytoin, carbamazepine, valproic acid, phenobarbital, clonazepam, primidone, and ethosuximide—are used widely in Asian countries [8]. Second-generation antiepileptic drugs, such as lamotrigine, gabapentin, tiagabine, felbamate, vigabatrin, or topiramate, are used widely in Malaysia, China, and Singapore and in some of the economically less developed countries, including the Philippines and Vietnam [9]. Common drugs used to treat epilepsy and their side effects are listed in Table 3.
Some people whose seizures are unmanageable with AEDs may benefit from VAGUS NERVE STIMULATION with a Neurocybernetic Prosthesis (NCP). The FDA approved the use of VNS in 1997. It is approved as an adjunct therapy for refractory partial seizures in adults and adolescents who are over 12 years old [10].
Surgery is another treatment option for patients who are refractory to AEDs or have seizures or side effects that significantly impair their quality of life. They must also be between 12 and 50 years old [11]. Several studies document the longer the patient has epilepsy prior to surgery the greater the relapse risk and they are more likely to have postsurgical auras [12]. There are four widely accepted surgical procedures: focal resection, corpus collosotomy, hemispherectomy, and the multiple subpial transaction [11].
It has been known since biblical times that fasting decreases seizures for some individuals. The ketogenic diet (KD) was devised during the 1920s to simulate some of the metabolic effects of starvation. The diet is high in fat, adequate in protein, and allows minimal carbohydrates in a ratio of 3 to 4 g of fat : 1 g of combined protein and carbohydrate. The body is forced to metabolize fat rather than carbohydrate [13]. The KD appears to raise the seizure threshold in the brain but the mechanism is unclear at this time. Ketogenic diet may decrease seizure frequency up to 50% [14]. Most effective in children younger than ten years of age who do not respond to or cannot tolerate the side effects of AEDs [14]. This type of therapy has limited use because it has various complications including dehydration, gastrointestinal disturbances, hypertriglyceridemia, hypercholesterolemia, hypoproteinemia, infectious diseases, hepatitis, acute pancreatitis, persistent metabolic acidosis, osteopenia, renal stones, poor growth, and weight loss [15]. Therefore, this diet should be followed only under medical supervision.
There is little in the dental literature regarding the implications of seizure disorders on oral health and delivery of dental care. Dentofacial trauma occurring during seizures has been reported to include injuries to the tongue, buccal mucosa, facial fractures, avulsion, luxation or fractures of teeth, and subluxation of the temporomandibular joint [16]. A long-recognized AED side effect is the gingival hyperplasia reported to occur in up to 50% of patients treated with phenytoin. and also been reported to occur with sodium valproate and ethosuximide [17]. Other AED-related oral findings include recurrent aphthous-like ulcerations, gingival bleeding, hypercementosis, root shortening, anomalous tooth development, delayed eruption, and cervical lymphadenopathy [18]. Of particular interest to the orthodontist is a recent report of facial and body asymmetries affecting 41% of patients with partial seizures in the population studied; asymmetries included both hemihypertrophy and atrophy [19].
• Take complete health history
• List medications patient is taking. Look them up so you know their effects, side effects, potential for drug interaction, and any specific oral effects.
• Schedule proper frequency of oral hygiene and provide good oral hygiene instruction to ensure healthy periodontal tissue and health.
• Insure proper dental lightening (no lights directly in eyes). dark or colored glasses can be used as eye protection.
• Insure medications have been taken properly relative to dental appointment to minimize the risk of seizure.
• Perform proper periodontal and surgical treatment of gingival hyperplasia to minimize damage to teeth and supporting structures and to maintain proper aesthetics.
• The use of conscious sedation and general anesthesia is not contraindicated in patients with epilepsy. In some situations nitrous oxide or intravenous sedation may be necessary to safely and effectively provide dental care [10].
Most seizures do not constitute an emergency. But if the seizure has any of the characteristics of those listed below, then it does constitute an emergency and medical help needs to be rendered and/or summoned.
• A seizure that continues for more than 5 minutes without the patient gaining consciousness between the attacks (status epilepticus)
• Breathing difficulties after a seizure
• Persistant confusion or unconsciousness for more than 5 minutes
• Inzuries sustained during a seizure
• A first seizure
Patients with epilepsy and a malocclusion should have a comprehensive orthodontic evaluation. Adverse side effects of AEDs and past dental trauma should be researched by the orthodontist and reviewed as part of patient informed consent. Mechanical challenges such as closing interdental spaces in the presence of gingival hypertrophy should be considered when estimating treatment time. As part of the informed consent process, the possibility of soft-tissue injury during a breakthrough seizure is to be stressed. The metal in a fixed orthodontic appliance may distort images obtained by magnetic resonance imaging (MRI). When cranial MR scans are conducted at 1.5 T, stainless steel brackets cause significantly more distortion in cranial MR images than plastic, ceramic, or titanium brackets [20]. Patients with poorly controlled seizure disorders that manifest with falling and/or uncontrolled body movements are not candidates for any type of orthodontic appliance.
Patients with seizure disorders face discrimination and difficulties in many aspects of their lives.21 The orthodontic team should be prepared to offer these individuals the care, consideration, and benefits of orthodontic treatment. Education of all members of the orthodontic staff about seizure disorders and their management, including office medical emergency drills, will lead to confidence and a positive attitude about including these patients in orthodontic practice.