e-ISSN: 2320-7949 and p-ISSN: 2322-0090
e-ISSN: 2320-7949 and p-ISSN: 2322-0090
Department of OBGY DR V M MC Medical Collage, Solapur, Maharashtra, India.
Received: 31/07/2014 Revised: 19/08/2014 Accepted: 30/08/2014
Visit for more related articles at Research & Reviews: Journal of Dental Sciences
To study the maternal view regarding pain relief, neonatal outcome, labour outcome under epidural anesthesia and to study the duration of various stages of labour and progress of labour under epidural anesthesia The present study comprises of continuous lumbar epidural analgesia with Bupivacaine (0.125%) pain relief during labour, carried out at Obstetrics and gynecology Department in collaboration with Anesthesiology Department of a Teaching General Hospital. A total of 100 cases (primigravidas) were studied out of 50 received continuous lumbar epidural analgesia and 50 served as control. There is an association between epidural analgesia and labour outcome, but this is probably not causative. In present study incidence of LSCS is 8%. In present study also there is no significant difference between caesarean delivery rates in group A (epidural group) and group B (control group). In our study there was no statistical difference in the duration of the active-first and the second stages of labor in both groups. In our study, the cesarean delivery as well as vacuum-assisted and instrumental delivery rates was not significantly different between both the groups. Epidural analgesia is highly effective and safe for both mother and foetus during labour. .It is proved to be effective in reducing pain, has no significant impact on the risk of cesarean section, maternal satisfaction is high, and does not have effect on the neonate.
epidural analgesia, maternal, neonatal
The pain of child birth is arguably one of the most severe types of pain a woman will endure in her life time. No woman should be denied of pain relief during labour. Relief of labour pain has always been controversial Labour and delivery is amongst the most painful of human experiences. Women have been able to cope up with this pain with these extreme conditions probably in anticipation of the result and the passage of years and that the happy experiences of motherhood dull the memories of pain. Pain in labour was thought to be essential to the birth process until mid nineteenth century. The idea of eliminating pain from natural childbirth was thought to be inappropriate and dangerous. Child birth should be pleasant and painless experience in human being. The desire to improve patient care and safety continues to be one of the primary goals and challenges for those providing obstetric analgesia services. Epidural analgesia possesses a long record of safety and has few complications and has evolved to be considered as “GOLD STANDARD” for pain relief during labour. Every doctor practicing obstetrics must have a wide knowledge of various drugs and techniques that may be used to achieve safe and effective pain relief. In present study we have tried to asses’ effect of Epidural analgesia on course of labour and to evaluate adverse effect on mother and fetus.
The present study comprises of continuous lumbar epidural analgesia with Bupivacaine (0.125%) pain relief during labour, carried out at Obstetrics and gynecology Department in collaboration with Anesthesiology Department of a Teaching General Hospital. A total of 100 cases (primigravidas) were studied out of 50 received continuous lumbar epidural analgesia and 50 served as control.
Selection Of Patients
Following criteria were used for selection of patients:-
• The full term (37-40wks) primigravida patient willing for continuous / single shot lumbar epidural analgesia.
• The Presentation vertex and spontaneous vaginal delivery expected.
• The patient in active labour (cervical dilatation more than > 3 cm.)
The contraindication for epidural blockade considered were as follows:-
• The patient not willing for epidural analgesia.
• Abnormal presentation.
• Previous LSCS.
• Cephalopelvic disproportion.
• Antepartum hemorrhage / Hypotension
• Coagulation disorders.
• Spinal deformity.
• Local sepsis at the site of puncture and systemic sepsis.
• Known case of sensitivity of local anesthetic agent.
• Fetal distress.
The patients were divided into two groups as –
Group A : 50 patients who received epidural analgesia.
Group B : 50 patients who served as control
The procedure was explained to the patients in brief. A written consent was taken to receive epidural analgesia. After explaining the process and getting informed written consent, the patient was asked to empty the bladder. Intravenous line secured to facilitate immediate rapid infusion or fluid in case of a fall in BP. The epidural catheter was placed at the L2-3 or L3-4 interspace. BP, HR and SpO2 were monitored and the visual analogue pain scores (VAS, 0-100 mm scale: 0= no pain, 100 = worst pain ever) were recorded before the block. The patients were shown a 10cm long horizontal scale marked from 0-10cm on a blank piece of paper and told to assess her pain. Scores ≤3were considered satisfactory. When the women who were receiving an epidural infusion, complained of pain, a 5 ml of bolus of anesthetic solution was given. Total number of boluses required during the 1st &2nd stage of labour was recorded. Uterine contractions and fetal heart rate (FHR) were monitored by an external cardiotocograph monitor. Fetal condition was also monitored and evidence of fetal distress, on clinical and/or cardiotocographic monitoring, was recorded.
Quality of analgesia was judged as
- Excellent - Complete relief experienced.
- Satisfactory - Pain relief is there but some pain experienced.
- Inadequate Slight pain relief experienced but pain experienced during most of time.
- No pain relief at all.
Assessment of pain relief – By VISUAL ANALOGUE SCALE- Perception of pain relief is subjective and this variable was standardized by using data from Visual analogue scale.
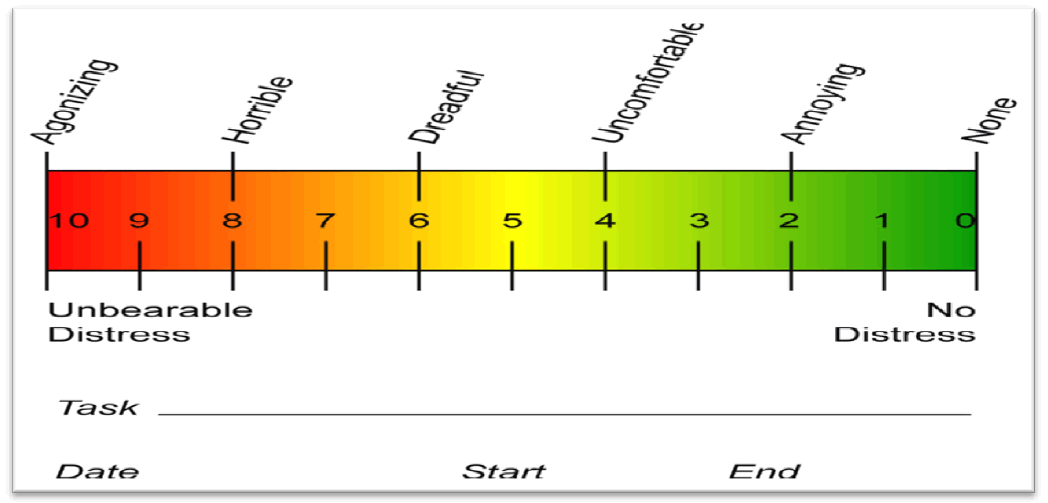
Visual Analogue scale involves the use of 10cm scale which was marked from 0-10. This was explained to the parturient that one end of the scale with red represents as much pain as much she can possibly imagine while the other end colored green represents no pain at all. The subject rates the degree of pain by the colour on the visual analogue scale. Values are then obtained from the scale.
VAS before epidural analgesia
VAS at 5 min , 10 min ,20 min , 30 min, 45 min, 60 min, and after that half hourly till delivery of baby . Mean VAS is calculated for 1st and 2nd stage of labour.
Motor power was assessed using a modified Bromage score at hourly intervals and at each request to get out of bed.
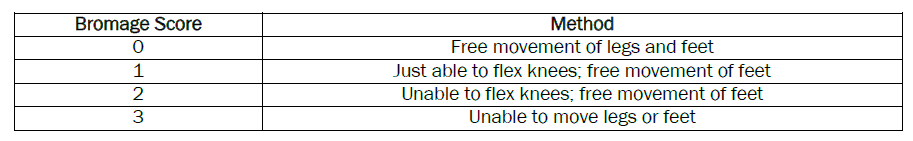
The degree of motor block was assessed according to a modified Bromage scale before administration of epidural analgesia and 5, 10, 20, 30 45, 60 min after the first dose of drugs, and every 30 min thereafter until delivery.
If the patients did not receive adequate pain relief within 30 minutes of first dose, 5 ml of the test solution was repeated at minimum intervals of 5 minutes till adequate analgesia was established. Analgesia was measured using visual analogue scores on a 100mm scale. After the initial dose of the test drug, visual analogue scale was measured at the peak of each contraction and the time of onset of first painless contraction noted. The establishment of epidural blockade was tested with skin prick using a needle and the time taken for loss of sensation to pinprick was also noted. Measurements were performed every 30 min. until delivery. The target for adequate analgesia is said to be attained when visual analogue score is less than 30 mm. The VAPS and the highest dermatomal level of sensory block were assessed using loss of sensation to pinprick was measured before administration of epidural analgesia and 5, 10, 20, 30, 45, 60 min after the first dose of drugs, and every 30 min. thereafter until delivery. Patients who required instrumental delivery received 10 ml of the test solution before the procedure in sitting position. Patients who required cesarean section received the test solution till T4 level were achieved.
Mode of delivery was recorded, as were duration of first and second stages of labour and time from insertion of the epidural until delivery. Fetal heart rate was monitored.Complications related to epidural, like dural puncture and venous puncture were looked for. Complications due to drugs like hypotension defined as a decrease of more than 20% of initial baseline value, pruritis, nausea/vomiting, drowsiness/sedation, rigor, urinary retention and respiratory depression were determined and recorded.
Show background data of women in two groups. There is no significant difference in two groups with regard to age, height, parity, weight and gestational age.
Table 2 and 3 Shows comparison of duration of first stage and second stage of labour in two groups respectively. There is no significant p value in both groups.
Table 4 shows comparison of obstetric outcome in both groups In present study also there is no significant difference between caesarean delivery rates in group A (epidural group) and group B (control group).Epidural analgesia do not increases rate of caesarean delivery.
Table 5 revales that incidence of fetal distress ,non progressive of 2 nd stage, instrumental delivery were not statisticallly difference in two groups.
On analyzing neonatal outcome it has been seen that there is no statistically significant difference in APGAR score in both groups
Basal pain intensity defined as the intensity of the pain assessed just prior to the block, has been measured with a 10 cm visual analogue scale (VAS).
Excellent: When mother was completely pain free from the first or second injection until end of delivery.
Good: When mother was satisfied but some pain was experienced for a short period during labour or delivery.
Incomplete: When mother had significant pain relief, but experienced some pain during most of the time of labour and delivery.
Failure: When after the start of epidural analgesia, pain was experienced during most of labour and delivery.
In the present study majority of women 60% felt their experience as better than expected i.e. excellent and 38% women felt it to be as expected i.e. satisfactory. Only 2% patients had incomplete analgesia
In the present study maximum patients had their Bromage score 0.
Table 11 shows unintended side effect of epidural analgesia. In the study hypotension and compensatory tachycardia was seen in 2% patients
In present study no other complications were observed such as high epidural, dural tap, accidental intravenous or intrathecal injection of drug, infection or epidural hematoma. No neurological squeal in the form of backache, headache or urinary disturbance was found during hospital stay. The catheter was removed completely and easily in all patients.
Superior quality of pain relief obtainable with regional analgesia in comparison with narcotic analgesic drugs is indisputable [1,2,3], and long periods of pain relief with minimal disturbance of labour pain can be obtained by epidural analgesia. Various concentration of different drugs like lignocaine, mepivacaine, ropivacaine, carbocaine, bupivacaine etc. have been tried for injection into epidural space for pain relief in labour [4,5,6]. The first report which appeared in literature using bupivacaine for epidural analgesia was done by E. K. Blom & Widman in 1964 [7]. Since then, the discovery of bupivacaine, many studies have been carried out for painless labour using other drugs. But the accuracy of results are not easy to evaluate, since the clinical situation, method of evaluation vary from centre to centre [8].
For the present study 0.125 % bupivacaine was used to study the efficacy of epidural analgesia during labour [9,10,11]. There is an association between epidural analgesia and labour outcome, but this is probably not causative. In present study incidence of LSCS is 8%. RCT conducted by Philipsen and Jensen 1989 [12], Sharma et al 1997 [13], Bofill et al 1998 [14] ,Clark and Colleagues 1998 [15] ,showed no significant difference between caesarean delivery rates associated with epidural analgesia as compared to those without epidural analgesia. In present study also there is no significant difference between caesarean delivery rates in group A (epidural group) and group B (control group). Though women who receive epidural analgesia during labour are more likely to require instrumental or caesarean delivery, there is little evidence to suggest that the epidural itself is to blame.
In our study there was no statistical difference in the duration of the active-first and the second stages of labor in both groups. In our study, the cesarean delivery as well as vacuum-assisted and instrumental delivery rates was not significantly different between both the groups.
The mechanisms whereby regional analgesia might affect the condition of the foetus at birth includes:-
• Alteration in placental blood flow.
• Alteration in uterine contractions and tone.
• Direct action of local anesthetics on the foetus.
• Alteration in maternal respiration and acid-base balance.
• Relaxation of pelvic floor muscle.
• Provision of optimal conditions for controlled delivery.
Note all of these mechanisms are necessarily harmful to the foetus. Some are undoubtedly beneficial [16]. Whatever may the risk/benefit ratio to the mother, all the evidence suggests that, provided the maternal circulation is well maintained, epidural analgesia in labour is actually beneficial to the baby, and that of the local anesthetics in current use bupivacaine would appear the most favorable [17].
The use of epidural Bupivacaine, with its reduced placental transfer, has not been associated with neonatal muscle tone and neurobehavioral responses were normal. 18 A direct pharmacological effect on the foetus and newborn is more likely to occur with epidural than with spinal administration, since the dose used by the later route is small. Moreover, although a direct effect may occur with the more cumulative lignocaine, it appears unlikely with Bupivacaine In the present study group A 4% patients and group B 2% patients had meconium stained liquor.
Hypotension and compensatory tachycardia was seen in 2% patients. Earlier, the incidence of this complication was almost 20%. The causes for development of hypotension with epidural analgesia are [16]:
• Supine position leading to caval occlusion
• Preganglionic sympathetic block with reduced peripheral resistance
• Hypovolemia resulting from blood loss and loss of other fluids.
Now in most of hospitals, the patients are kept in left lateral position during epidural analgesia in labour. We kept all the patients in left lateral position, preloaded adequately and kept IV maintenance fluids. These might be the reason for low incidence of hypotension in our study. Urinary retention is a known complication of child birth. Weil A [19] Ramsay and Torbet 1993 [20] who first studied epidural as a possible risk factor for urinary retention suggested that epidural analgesia could delay normal voiding by reducing a suppressing afferent sensory impulses from the bladder. Present study only 1 (2%) patient had urinary retention after delivery for that simple catheterization done and patients observed after 4 hrs patients regain her bladder control, no other extra intervention needed.
Although the association between epidural and hyperbilirubinemia is consistent, the reason for this association is not clear. Apart from the epidural itself, 2 other factors have been investigated as a possible explanation for the increase in bilirubin.
• Use of oxytocin
•Instrumental delivery
Both of them may be more likely with epidural analgesia.
Instrumental delivery represents a plausible mechanism because it has been associated with an increase in the occurrence of neonatal jaundice. In the present study 2% neonate had hyperbilirubinemia on postnatal day 2, but oxytocin was not used in these patients neither they were delivered instrumentally.
Epidural analgesia for pain relief in labor is accepted widely. In the present study majority of women 60% felt their experience as better than expected i.e. excellent and 38% women felt it to be as expected i.e. satisfactory. Only 2% patients had incomplete analgesia.
Epidural venous puncture was seen in 3 (6%) patients. This could be attributed to accidental dural venous puncture due to technical errors. None had any major complication. In present study 1 (2%) patient had back ache after delivery patient put on oral analgesic patient’s symptoms relieved. Epidural labour analgesia is associated with maternal fever. The exact mechanism is unknown; it may be result of increased heat production (e.g. shivering), decreased heat loss (inhibition of sweating secondary to neuroblockade or less heat loss via respiratory tract because of lack of hyperventilation) or alterations in temperature regulation induced by epidural analgesia. In present study 0% patient had pyrexia. Epidural related fever is generally believed to result from thermoregulatory alterations rather than infection In the present study maximum patients had their Bromage score 0.
In present study no other complications were observed such as high epidural, dural tap, accidental intravenous or intrathecal injection of drug, infection or epidural hematoma. No neurological squeal in the form of backache, headache or urinary disturbance was found during hospital stay.
Epidural analgesia is highly effective and safe for both mother and foetus during labour. .It is proved to be effective in reducing pain, has no significant impact on the risk of cesarean section, maternal satisfaction is high, and does not have effect on the neonate. The morbidity, mortality, and cost for women undergoing Cesarean delivery are greater than for women who have a vaginal delivery. Since epidural analgesia was introduced four decades ago for pain relief in labour, controversy has persisted about its effect on the labour process. Epidural analgesia may be associated with an increased risk of cesarean delivery for dystocia although a cause and effect relationship has not been proven. Similarly, pain is associated with dystocia but is not the cause .As a result of this, considerable research has been performed and findings have led to changes in practice. Epidurals have been credited with prolonging labour; increasing oxytocin requirements, instrumental and operative delivery rates; and causing maternal pyrexia and postpartum back pain. There is increasing evidence that refuses some of these claims.