Nanosensors Success in Cardiovascular Diseases
Kiran Mayee K1* and Mahesh G2
1Department of Pharmaceutical Analysis, Malla Reddy College of Pharmacy, Telangana, India
2Department of Pharmacy, Anurag Group of Institutions, Telangana, India
- *Corresponding Author:
- Kiran Mayee K
M. Pharmacy, Department of Pharmaceutical Analysis
Malla Reddy College of Pharmacy, Telangana, India.
E-mail: kondabathinilight@gmail.com
Received date: September 02, 2016; Accepted date: September 05, 2016; Published date: September 12, 2016
Visit for more related articles at Research & Reviews: Journal of Pharmaceutics and Nanotechnology
Abstract
Nanotechnology is modest representation of tiny in meaning, but nanometer is one-billionth of a meter. A solitary walled carbon nanotube with a distance across of 1 nanometer is 100,000 times littler than a strand of hair. In examination, a strand of hair is 100,000 times littler than a house 10 meters wide. Nanotechnology is the future technology with immense scope for various applications, such as nanomedicine, nanoelectronics, nanaosensors, etc. Nanosensors are natural, synthetic, or surgical sensory point’s used to transfer information about nanoparticles to the macroscopic arena. For the most part utilized as a part of different therapeutic purposes and as passages to building different nanoproducts, for example, PC chips that work at the nanoscale and nanorobots. A typical notion that individuals have with nanotechnology inside the human body is whether the materials utilized are lethal. The sensors, developed from carbon nanotubes, are fit for detecting whether cells joining to the insert are bone cells (as would be trusted), microscopic organisms or provocative cells.
Keywords
Nanotechnology, Nanomedicine, Nanosensors, Cardiovascular diseases, Carbon tubes
Introduction
Cardiovascular Diseases
Cardiovascular diseases (CVD) are rapidly witnessed all over the world with a huge number of individuals and are expected to be continued as one of the top most indorsers to healthcare expenditure. According to WHO, approximately 17 million people’s lives have been snatched away by CVD each year throughout the world [1-7].
Generally six types of cardiovascular diseases are common & they are listed below:
• Ischemic heart disease
• Cerebrovascular disease (Stroke)
• Peripheral vascular disease
• Heart failure
• Rheumatic heart disease
• Congenital heart disease
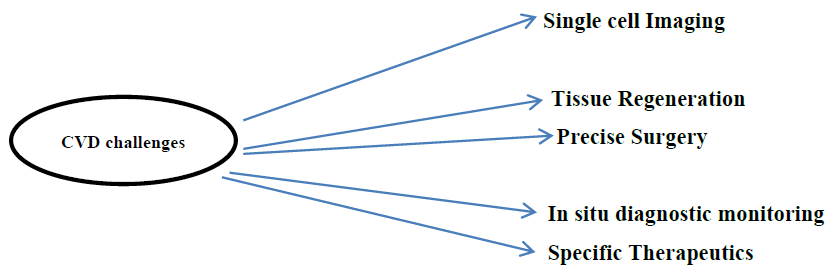
Challenges of CVD include
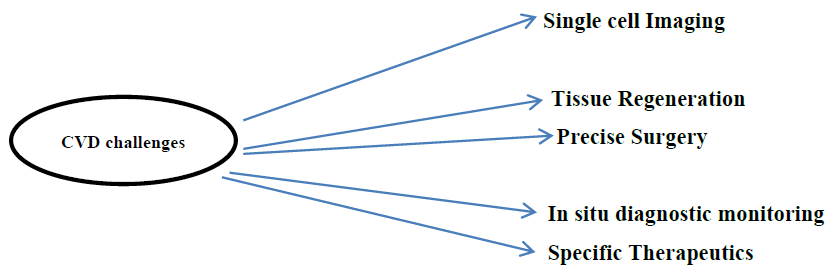
Nanosensors in Cardiovascular Diseases
Nanosensors in medicinal research are fast emerging, and particularly in heart ailments. Poor dietary examples and less dynamic lifestyles are the basic reasons for expanding Heart diseases & disorders. Cardiovascular diseases are sudden and needs rapid consideration and fast treatment. Nano sensors are designed such a way as to detect a heart attack by calculating the stress reaction in the heart and converting it into an ECG signal [8-10]. Nanosensors are able to wirelessly covey the signal to physicians for rapid diagnosis and treatment. These sensors are less cost and can be used by individuals with cardiac disease at all times.
Severe stress in the heart, leads to excess release of enzymes (protein molecules), thereby putting pressure and exertion on blood vessels; which leads to chest pain or cardiac arrest [11-35].
Nanosensors
Devices with nano arranged materials are used for both prior processing and sensing analysis. Two or three chips are being elaborated for use in medical monitoring or diagnostics. First chip is associated with analyte preliminary processing and sensing structures, it will be made by the nanofab created. Rest of the chips would be with standard microcontrollers. Nanosensors have a silicon or polymeric filters with nano sized sieving structures; micro liquid systems for bio-object sorting; a micro PCR; single chip electrophoresis system; a single chip (with outward light source) SPR system with microscale substance and catalytic sensors with deep submicron structures for better functionality and response time [36-40].
Various Projects of Successful Nanosensor in Cardiovascular Disease around the World
Approaches of Cardiovascular detection may be different, but ultimate goal is for proper diagnosis & better treatment of diseased individuals.
Testing C-reactive protein (CRP) levels in the blood
C-reactive protein is one of the critical phase proteins that elevate during inflammation. Increased levels of CRP continuously suggest recurrent coronary episodes in patients with unsteady angina and acute myocardial infarction (heart attack). Elevated CRP levels also are linked with lower survival rates in cardiac patients [41-47].
Portugal researcher’s developed a novel approach for treatment of CV disease based on a transducer array made of carbon nanotubes for the selective and sensitive assessing of C-reactive protein in blood and saliva. This non-invasive approach is a very less time taking and does not need any sample prior treatment analysis, it can provide immediate results in situ and therefore it will elevate the capacity of diagnostics in real time and as a result it will lead to improve the quality of health care systems [48-56].
Project is started firstly with assembling of nanosensor, tested and optimised for standard solutions. Nanosensor included by a transducer array made of single-wall carbon nanotubes on compatible oxides of metallic semiconductor with silicon substrate and chemical recognition layers or coatings that elevate the transducer´s sensitivity and selectivity to the specific analytes. The nanosensor will be used to the detection of C-reactive protein in artificial samples and the results estimated with the ones obtained with ELISA assay [57-76].
Second step of project include, application of nanosensor to actual clinical samples (human blood and saliva) and the results will also be demonsrated using ELISA assay. Samples taken from human would be blood and saliva either from healthy individuals or individuals suffering from different diseases associated with C-reactive protein. Results acquired for saliva will be tested alongside blood in order to identify if C-reactive protein in saliva gave important result for cardiovascular risk disease and to check the nanosensor as a non-invasive technique.
Third step of project includes the nanosensor adjusted to a prototype and tested with real samples.
IIT Mumbai, Department of Electrical Engineering has developed a cantilever in the sensor using tiny or nano-particles of the polymer to measure the stress symptom (myocardial infarction) in the heart and change it into an electrical signal. Nano-particles, in a polymer produce electrical current through biochemical procedure of the enzymes produced in the heart. As the heart experiences intense stress or strain, it immediately releases enzymes (protein molecules) in bulk, exerting pressure on its blood vessels, which outcome as chest pain, perspiration or even a cardiac arrest.
Silicon Nanosensor technology depending on electrical impedance measurements was constructed for identification of proteins. The nanosensor miniaturizes the high-density, low-volume multiwell plate concept. Estimation of two cardiac proteomic biomarkers has been established through this technology. Ttwo proteins, C-reactive protein and NT-pro-brain natriuretic peptide (BNP), are associated with adverse cardiac consequence in clinical samples when analysed in the pg/mL concentration. Occurrence of the antibody-antigen binding complex in individual wells is noticed. This technology has the capability to achieve near real-time detection with improved sensitivity at 1 ag/mL for BNP and 1 fg/mL for CRP from human serum.
Rapid multi-channel serum profiling for cardiac disease
Rapid Multi-Channel Serum Profiling for Cardiovascular disease was performed by researchers from USA.
Fluorescent Nanosensors fastens the diagnosis of cardiac aliments in individuals with CV Diseases, minimizing economic impact. Proposed research uses nanoparticle-based sensor arrays to quickly profile serum, highlighting on the creation of effective sensor elements that use supramolecular "hairpin" motifs to provide a turn-on fluorescence response. Covalent bonding of the nanoparticle recognition element and fluorescent reporter will permit their use in flow systems.
Conclusion
Expansion and current understanding of various sectors in molecular biology [77-79], material science, genetics, cellular biology, bioengineering [80-85] and proteomics [86-97] develop nanobiotechnology. Nanobiotechnology [98-100] acts as a bridge between interactions on the microscopic and molecular levels, leading a path for outstanding and inclusive platform from where it can become the important prospective towards the progress of CVD diagnosis and treatment.
References
- Magomedova SA and Damadaeva AS. Medico-Social and Psychological Aspects of Cardiovascular Diseases. Biol Med (Aligarh). 2016;8:332.
- Zafar R. An Insight into Pathogenesis of Cardiovascular Diseases. J Cardiovasc Dis Diagn. 2015;3:197.
- Hanefeld M, et al. The Metabolic Syndrome and Cardiovascular Diseases: An Update of Medical Treatment. J Metabolic Synd. 2014;3:160.
- Patel NKJ, et al. Metabolic Syndrome and its Impact on Cardiovascular Diseases. J Metabolic Synd. 2014;3:142.
- Zafar R. A New Insight into Pathogenesis of Cardiovascular Diseases: Stress Induced Lipid Mediated, Vascular Diseases. J Cardiovasc Dis Diagn. 2015;3:206.
- Izumi Y. Therapeutical Potential of Microvesicles in Cardiovascular Diseases. J Genet Syndr Gene Ther. 2012;3:e107.
- Afroz R, et al. Honey-derived Flavonoids: Natural Products for the Prevention of Atherosclerosis and Cardiovascular Diseases. ClinExpPharmacol. 2016;6:208.
- Omar HR, et al. Delayed Cath- Lab Activation for STEMI Due to Erroneous Computer Electrocardiogram Interpretation: A Note of Caution for Emergency Physicians. Emergency Med. 2016;6:306.
- Dodo-Siddo M, et al. Importance of Electrocardiogram for Detection of Preclinical Abnormalities in Patients with Rheumatoid Arthritis without Cardiovascular Events. J Arthritis. 2015;4:155.
- Cimen A, et al. Demonstration of Early Endothelial Dysfunction in Diabetics with Normal Exercise Electrocardiogram. Int J Cardiovasc Res. 2014;3:4.
- Agarwal V, et al. Extensive Coronary Disease in a 24 year Old Woman without Traditional Risk Factors Presenting as Cardiac Arrest. J Womens Health, Issues Care. 2014;3:3.
- Gardner G and MacDonald S. Neuromuscular Blocking Agents and Therapeutic Hypothermia Post Cardiac Arrest in the Intensive Care Unit: Knowledge to Practice. AnalgResusc: Curr Res. 2014;3:2.
- Babbs CF. The Case for Interposed Abdominal Compression CPR in Hospital Settings. AnalgResusc: Curr Res. 2013;3:1.
- Dabbous AS, et al. Reflex Bradycardia and Cardiac Arrest Following Sigmoidoscopy under General Anesthesia. AnalgResusc: Curr Res. 2013;2:2.
- Wagner H, et al. A Structured Approach for Treatment of Prolonged Cardiac Arrest Cases in the Coronary Catheterization Laboratory Using Mechanical Chest Compressions. Int J Cardiovasc Res. 2013;2:4.
- Johnson D, et al. The Effects Vasopressin and Epinephrine on Cardiac Arrest Following Desipramine Overdose in a Porcine Model AnalgResusc: Curr Res. 2013;S1.
- Trabelsi W, et al. An Uncommon Cause of Cardiac Arrest. AnalgResusc: Curr Res. 2013;S1.
- Maccaroni MR, et al. Managing Cardiac Arrest after Cardiac Surgery: The Impact of a Five Year Evolving Re-Sternotomy Policy and a Review of the Literature. AnalgResusc: Curr Res. 2013;S1.
- Mayette M and Lighthall GK. The Impact of Continuous Patient Monitoring at Various Times of Day on In-hospital Cardiac Arrest Mortality. AnalgResusc: Curr Res. 2013;S1.
- Haris Bilal R, et al. Sole Abdominal Compression Cardiopulmonary Resuscitation: A Novel Technique in the Management of Cardiac Arrest Following Cardiac Surgery. AnalgResusc: Curr Res. 2013;S1.
- Johnson D, et al. Effects of the ResQPod® on Maximum Concentration and Time to Maximum Concentration of Epinephrine in a Porcine Cardiac Arrest Model. AnalgResusc: Curr Res. 2013;S1.
- Baker WL, et al. Effect of Neuromuscular Blockers on Outcomes in Patients Receiving Therapeutic Hypothermia Following Cardiac Arrest AnalgResusc: Curr Res. 2013;S1.
- Trabelsi W, et al. In-hospital Cardiac Arrest: How to Become a Good “Samaritan”? AnalgResusc: Curr Res. 2013;S1.
- Hernandez-Padilla JM. Prevention and Early Management of In-Hospital Cardiac Arrest: A Challenge for Nursing Educators. J Nurs Care. 2016;5:e132.
- Ogura K, et al. A Case of Successful Extracorporeal Membrane Oxygenation Support for Cardiac Arrest Associated with Non-occlusive Mesenteric Ischemia. Emerg Med (Los Angel). 2016;6:322.
- Parri SNF, et al.Unexpected Cardiac Arrest due to ExtrapericardialTamponade: Beware of Hemomediastinum!.Emerg Med (Los Angel). 2015;5:276.
- Johnson S and Nileswar A. Effectiveness of Modified Early Warning Score (MEWS) in the Outcome of In-Hospital Adult Cardiac Arrests in a Tertiary Hospital. J PulmRespir Med. 2015;5:285.
- Ortega-Deballon I. Cardiac Arrest, Resuscitation and Organ Donation: Joint Venture for Saving Lives One Way or Another. An Innovative and Ethically Sound Trail for Out-of-Hospital Cardiac Arrest. J Clin Trials. 2015;5:237.
- Anderson ML, et al. Cardiac Arrest and Cardiopulmonary Resuscitation (CPR) Knowledge at an Academic Research Organization in Durham, NC. Emerg Med (Los Angel). 2015;5:266.
- Curtis B, et al. Defecation Syncope: Two Cases of Post-Operative Cardiac Arrest. Anaplastology. 2015;4:142.
- Melanie Pittard, et al. Takotsubo Cardiomyopathy Induced Intraoperative and Postoperative Cardiac Arrests. J AnesthClin Res. 2014;5:454.
- Hassan N, et al. Improving Chest Compressions Following Cardiac Arrest: Pushing Ahead. J AnesthClin Res. 2014;5:390.
- Lenjani B, et al. Cardiac Arrest - Cardiopulmonary Resuscitation. Gen Med (Los Angel). 2014;2:131.
- Takeuchi N, et al.Nonocclusive Mesenteric Ischemia Resulting from Acute Myocardial Infarction of Left Main Trunk after the Recovery from Cardiac Arrest by Percutaneous Cardiopulmonary System: A Case Report. Intern Med. 2014;4:133.
- Copetti R. Clinical Integrated Ultrasound in Peri Cardiac Arrest and Cardiac Arrest. J Clinic Experiment Cardiol. 2013;S10:003.
- Choi D. Biosensors and Bioelectronics. Sensor Netw Data Commun. 2016;S1:e002.
- Lopez-Barbosa N and Osma JF. Biosensors: Migrating from Clinical to Environmental Industries. Biosens J. 2016;5:e106.
- Singh RP. Nanobiosensors: Potentiality towards Bioanalysis. J Bioanal Biomed. 2016;8:e143.
- Capineri L. Piezoresistive Sensors Fabricated with Conductive Textiles for Monitoring the Step Rate with Read-Out Electronics and Wireless Connection to a Smart Watch. J Fashion Technol Textile Eng. 2015;3:3.
- Girousi ST.Electrochemical Biosensors; A Promising Tool in Pharmaceutical Analysis. Pharm Anal Chem Open Access. 2016;2:e104.
- Mahato K, et al.Nanobiosensors: Next Generation Point-of-Care Biomedical Devices for Personalized Diagnosis. J Anal Bioanal Tech. 2016;7:e125.
- Das AP.Biosensors: The Future of Diagnostics. Sensor Netw Data Commun. 2016;S1:e107.
- Ko HJ. Recent Update of Nanobiosensors Using Olfactory Sensing Elements and Nanomaterials. BiosensJ. 2015;4:129.
- Gonzalez-Rodriguez J and Raveendran M. Importance of Biosensors. Biosens J. 2015;4:e104.
- Chandra P. Electrochemical Nanobiosensors for Cancer Diagnosis . J Anal Bioanal Tech 6:e119.
- Fang Y (2013) Biosensors: On the Origin of Label-Free Cell Phenotypic Profiles of Drug-Receptor Interactions. J Biochips Tiss Chips. 2015;3:e126.
- Menaa F. Graphene-Based Biosensors for Nano and Pico Applications: The Future is here! Pharmaceut AnalActa. 2013;5:e161.
- Broderick PA. Biosensors and Biochips Sense Central and Peripheral Disease. J Biochips Tiss Chips. 2013;3:e122.
- Vashist SK and Venkatesh AG. Carbon Nanotubes-Based Electrochemical Sensors and Drug Delivery Systems: Prospects and Challenges. J NanomedNanotechol. 2012;3:e121.
- Ramirez-Vickl JE. Nanostructured ZnO for Electrochemical Biosensors. J BiosensBioelectron. 2012;3:e109.
- Halamek J. Biosensors Technology. J Biochips Tiss Chips. 2012;2:e112.
- Carroll D and Alwarappan S. Recent Advances in Biosensors and Biosensing Protocols. J BiosensBioelectron. 2012;3:e112.
- Sirivisoot S and Webster TJ. Biosensors as Implantable Medical Devices for Personalized Medicine. J BiosensBioelectron. 2012;3:e104.
- Achyuthan K. Whither Commercial Nanobiosensors? J BiosensBioelectron. 2011;2:102e.
- Asif MH, et al.Electrochemical Biosensors Based on ZnO Nanostructures to Measure Intracellular Metal Ions and Glucose. J Anal Bioanal Tech. 2011;S7:003.
- Vijaya Krishna V. Biosensors. J Bioeng Biomed Sci. 2011;1:e101.
- Ma X, et al. Development of an Indirect-Elisa to Detect Antibodies against Porcine Reproductive and Respiratory Syndrome Virus Nucleocapsid Protein in Gansu China. J VirolAntivir Res. 2016;5:2.
- Priyadarshi SS, et al. Diagnosis of Cysticercosis in Eye and Treatment Follow-Up of Extra Ocular Forms by Serum IgGELISA. Int J Ophthalmic Pathol. 2015;4:1.
- Roda E, et al. Evaluation of Two Different Screening ELISA Assays for Synthetic Cathinones (Mephedrone/Methcathinone and MDPV) with LC-MS Method in Intoxicated Patients. J ClinToxicol. 2016;6:302.
- Yilma M and Mekonnen M. Competitive Enzyme Linked Immuno-Sorbent Assay (c-ELISA) Based Sero-Prevalence of Bluetongue Virus (BTV) on Small Ruminants in Selected Areas of Wolyita, Southern Ethiopia. Virol-mycol. 2015;4:148.
- Casini D, et al.A Rapid ELISA Method to Improve the Automated Test Throughput. J Anal Bioanal Tech. 2015;S13:005.
- Biswas S and Saha MK. Uncertainty of Measurement for ELISA in a Serological Testing Laboratory. ImmunochemImmunopathol: Open Access. 2015;1:109.
- Afayoa M, et al. Development and Evaluation of an Antigen Capture Enzyme-Linked Immunosorbent Assay (AC-ELISA) the Diagnosis of African Swine fever. Virol-mycol. 2015;4:145.
- Meulenberg EP. The Development and Application of ELISA for 3-Indole-Butyric Acid. ImmunochemImmunopathol: Open Access. 2015;1:104.
- Du P, et al. Comparisons of VLP-Based ELISA, Neutralization Assays with Native HPV, and Neutralization Assays with PsV in Detecting HPV Antibody Responses in HIV-Infected Women. J AIDS Clin Res. 2015;6:433.
- Breuninger S, et al. Quantitative Analysis of Liposomal Heat Shock Protein 70 (Hsp70) in the Blood of Tumor Patients Using a Novel Liphsp70 ELISA. J Clin Cell Immunol. 2014;5:264.
- Farid AH and Segervall. A Comparison between ELISA and CIEP for Measuring Antibody Titres against Aleutian Mink Disease Virus. Virol-mycol. 2014;3:137.
- Erhabor O, et al. Comparison of ELISA and Rapid Screening Techniques for the Detection of HBsAg among Blood Donors in UsmanuDanfodiyo University Teaching Hospital Sokoto, North Western Nigeria. J Blood Lymph. 2014;4:124.
- Ramesh Kumar K, et al. Anti-Human IgG-Horseradish Peroxidase Conjugate Preparation and its Use in ELISA and Western Blotting Experiments. J Chromatograph SeparatTechniq. 2014;5:211.
- Wang F, et al. The Comparison of Chemiluminescent- and Colorimetric-detection Based ELISA for Chinese Hamster Ovary Host Cell Proteins Quantification in Biotherapeutics. J Bioprocess Biotech. 2013;3:136.
- Svobodova Z, et al. Dot-ELISA Affinity Test: An Easy, Low-Cost Method to Estimate Binding Activity of Monoclonal Antibodies. J Anal Bioanal Tech. 2013;4:168.
- Ribeiro D, et al. Subclinical Diagnosis of Caseous Lymphadenitis Based on ELISA in Sheep from Brazil. J BacteriolParasitol. 2013;4:170.
- Sasani F, et al.The Relationship between Microscopic Lesions and Different Types of Clostridium perfringens and their Related Toxins by Sandwich ELISA in Cattle. J MicrobBiochem Technol. 2013;5:034-038.
- Zhang Y, et al. Rapid Detection of Sporotrichosis by ABC-ELISA. J ClinExpDermatol Res. 2012;3:162.
- Wilson DJ, et al. Bovine Viral Diarrhea Milk ELISA Test Detecting Anti-p80 Antibody – Association with Milk Handling Methods and Cow Characteristics. J VeterinarSci Technol. 2012;3:114.
- Kitamura K, et al. Peptide Aptamer-Based ELISA-Like System for Detection of Cathepsin E in Tissues and Plasma. J MolBiomarkDiagn. 2011;2:104.
- Bhadra U, et al. Get Well in the RNAi Way-RNAi, A Billion Dollar Baby in Therapy. Mol Biol. 2016;5:158.
- Bhadra U, et al. RNA Interference (RNAi) as a metronome of the circadian cadence. Mol Biol. 2016;5:166.
- Hao Y, et al. miR-146a is Upregulated During Retinal Pigment Epithelium (RPE)/Choroid Aging in Mice and Represses IL-6 and VEGF-A Expression in RPE Cells. J ClinExpOphthalmol. 2016;7:562.
- Nwankwo N. Computer-Aided Drug Potency Decoder: A Biomedical/Bioengineering Device for Determining and Distinguishing Drug Efficacies. J Bioengineer & Biomedical Sci. 2015;6:176.
- Al-Kasasbeh RT, et al. Bioengineering System for Prediction and Early Prenosological Diagnostics of Stomach Diseases based on Energy Characteristics of Bioactive Points with Fuzzy Logic. J BiosensBioelectron. 2015;6:182.
- Brafman DA. Bioengineering of Stem Cell Microenvironments Using High-Throughput Technologies. J Bioeng Biomed Sci. 2012;S5:004.
- Roy P. Emerging Techniques in Bioengineering. J Bioeng Biomed Sci. 2012;S5:e001.
- Masumoto H and Keller BB. Bioengineering for Stem Cell-Based Cardiac Regeneration. J Stem Cell Res Ther. 2014;4:200.
- Luo Y. Bioengineering and Biomedical Science. J Bioeng Biomed Sci. 2014;4:e120.
- Shukla HD. Novel Genomics and Proteomics Based Biomarkers to Predict Radiation Response and Normal Radiotoxicity in Cancer Patients for Personalized Medicine. J Cancer Clin Trials. 2016;1:117.
- Simonian M. Proteomics in Medicine. J Data Mining Genomics Proteomics. 2016;7:e126.
- Mittal P and Jain M. Proteomics: An Indispensable Tool for Novel Biomarker Identification in Melanoma. J Data Mining Genomics Proteomics. 2016;7:204.
- Heidari A. Pharmacogenomics and Pharmacoproteomics Studies of Phosphodiesterase-5 (PDE5) Inhibitors and Paclitaxel Albumin-stabilized Nanoparticles as Sandwiched Anti-cancer Nano Drugs between Two DNA/RNA Molecules of Human Cancer Cells. J Pharmacogenomics Pharmacoproteomics. 2006;7:e153.
- Heidari A. Genomics and Proteomics Studies of Zolpidem, Necopidem, Alpidem, Saripidem, Miroprofen, Zolimidine, Olprinone and Abafungin as Anti-Tumor, Peptide Antibiotics, Antiviral and Central Nervous System (CNS) Drugs. J Data Mining Genomics & Proteomics. 2016;7:e125.
- Wright JC and Choudhary JS. DecoyPyrat: Fast Non-redundant Hybrid Decoy Sequence Generation for Large Scale Proteomics. J Proteomics Bioinform. 2016;9:176-180.
- Morris JA. Re-Discovering the Germ Theory of Disease: A Major Role for Proteomics. J Proteomics Bioinform. 2016;9:084-086.
- Bo-Yeong C, et al. Proteomics based Development of Biomarkers for Prion Diseases. J Proteomics Bioinform. 2016;9:087-100.
- Gamberi T, et al. Using Proteomics to Understand Abdominal Aortic Aneurysms: Where Are We? J Proteomics Bioinform. 2016;9:120-130.
- Noronha MA, et al. Developments in Cardiovascular Proteomics. J Proteomics Bioinform. 2016;9:144-150.
- Dubey R and Bhushan R. Replacement of “Amide Chemistry” with “Click Chemistry”: Current Trend in Proteomics. Organic ChemCurr Res. 2015;4:139.
- Lippolis R and De Angelis M. Proteomics and Human Diseases. J Proteomics Bioinform. 2016;9:063-074.
- Anderson DS, et al. Nanotechnology: The Risks and Benefits for Medical Diagnosis and Treatment. J NanomedNanotechnol. 2016;7:e143.
- Maroof K, et al. Scope of Nanotechnology in Drug Delivery. J BioequivAvailab. 2016;8:001-005.
- Patel S, et al. Nanotechnology in Healthcare: Applications and Challenges. Med chem. 2015;5:528-533.