e-ISSN: 2347-7857 p-ISSN: 2347-7849
e-ISSN: 2347-7857 p-ISSN: 2347-7849
Bharathisha BS1*, Prasanna Sagar2, SB Puranik3, Swamy Sreenivasa4, and Madhu Chakrapani Rao5
1Research Scholar, Bundelkhand University, Jhansi, Madhya Pradesh, India.
2Gland Pharma Pvt Ltd, Hyderabad, Andhra Pradesh, India.
3East West College of Pharmacy, Bangalore, Karnataka, India.
4Prof. C. N. Rao Center for Advanced Materials, Department of Chemistry, Tumkur University, Tumkur-572 103, Karnataka, India.
5Tadimety Aromatics Pvt. Ltd, Hirehally Industrial Area, Tumkur-572168, Karnataka, India.
Received date: 10/01/2014 Revised date: 20/02/2014 Accepted date: 28/02/2014
Visit for more related articles at Research & Reviews: Journal of Pharmaceutics and Nanotechnology
The recent trend or expansion of antifungal drug research has demonstrated that there is a critical need for new antifungal agents to treat these life-threatening invasive infections. Invasive fungal infections are the critical in treating immunocompromised patients. The overview of the development of antifungal therapy discussed in this article reflects the increased interest in this area of infectious diseases. Although newer, less toxic, antifungal agents are available for clinical use, their clinical efficacy in some invasive fungal infections, such as aspergillosis and fusariosis, is not optimal. Thus, intense efforts in antifungal drug discovery are still needed to develop more promising and effective antifungal agents for use in the clinical arena.
Antifungal agents, Therapy, Pharmacology, New targets
Fungi are heterotrophic organisms which are able to reproduce sexually as well as asexually. About 100 infectious fungal agents have been detected in man. Although the existence of fungi dates back a billion years, the history of medical mycology and human mycoses as reviewed by Espinel-Ingroff began in the early 19th century in Italy with the discovery of tinea favosa [1].
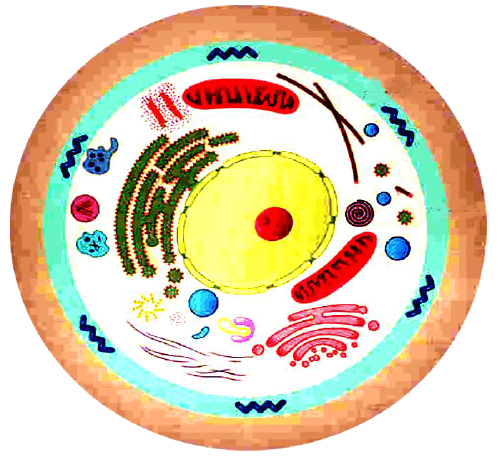
Pathogenic fungi are fungi that cause disease in humans or other organisms. The study of pathogenic fungi is referred to as "medical mycology." Although fungi are eukaryotic organisms, many pathogenic fungi are also microorganisms [2].
The mycoses or fungal infection can be of various forms as:
• Superficial – seen on the skin, the hair, and nails.
• Subcutaneous – infection reaching dermis or subcutaneous tissue
• Systemic – internal organs infected deeply
• Opportunistic – infection in immunocompromised patients
Pathogenic fungi cause disease in humans or other organisms. The study of pathogenic fungi is referred to as medical mycology. Pathogenicity is an accidental phenomenon and is not essential to the survival or dissemination of the fungal species involved. Most infections are either completely asymptomatic or of very short duration and quickly resolved.
Types of fungal infections – Mycoses
Superficial mycoses
Affect the skin, hair and nails
Subcutaneous mycoses (tropical)
Affect the muscle and connective tissue immediately below the skin
Systemic (invasive) mycoses
Involve the internal organs
Primary vs. opportunistic
Allergic mycoses
Affect lungs or sinuses
Patients may have chronic asthma, cystic fibrosis or sinusitis. Initial efforts at antifungal therapy were unsuccessful until the demonstration that a saturated solution of potassium iodide (SSKI), taken orally as drops, had some benefit in cutaneous sporotrichosis[3]. Unfortunately, use of SSKI was limited by its very narrow antifungal spectrum activity. As recognition of fungal infections increased, so too did the need for intravenous (IV) or oral antifungal agents. The first landmarks in the development of active and safe antifungal agents were the discovery of the antifungal activities of griseofulvin by Oxford, in 1939, and the first azole,benzimidazole, by Wooley in 1944[4,5,6]. Elson’s report on the fungistatic properties of propamidine followed in 1945[7] .This was followed by Hazen & Brown’s subsequent discovery of the first polyene macrolide antifungal, nystatin, in 1950, which had important implications for the modern era of antifungal therapy [8,9,10].
In 1951, propamidine and a related compound stilbamidine were used in a few human cases of blastomycosis with limited success, but with notable toxicity [10] .Two years later a less toxic stilbamidine derivative, 2-hydroxystilbamidine, was used in three additional human cases of blastomycosis, with limited success [11]. The discovery of amphotericin B (AmB) in 1955 and subsequent reports of its use to treat a several human cases of blastomycosis in 1957 illustrate the speed with which the search for effective and safe antifungal agents was progressing [12,13].
The introduction of oral griseofulvin and topical chlormidazole in 1958 and the subsequent introduction of IV AmB in 1960 heralded the beginning of the modern era of antifungal therapy [4]
What are the targets for antifungal therapy?
Cell membrane
Fungi use principally ergosterol instead of cholesterol: DNA Synthesis
Some compounds may be selectively activated by fungi, arresting DNA synthesis.: Cell Wall Unlike mammalian cells, fungi have a cell wall.
Cell Membrane Active Antifungals
Cell membrane:
Polyene antibiotics
Amphotericin B, lipid formulations, Nystatin (topical)
Azole antifungals
Ketoconazole, Itraconazole, Fluconazole, Voriconazole, Miconazole, clotrimazole (and other topicals)
Azoles – Mechanism
In fungi, the cytochrome P450-enzyme lanosterol 14-a demethylase is responsible for the conversion of lanosterol to ergosterol
Azoles bind to lanosterol 14a-demethylase inhibiting the production of ergosterol. Some cross-reactivity is seen with mammalian cytochrome p450 enzymes
Azoles bind to lanosterol 14a-demethylase inhibiting the production of ergosterol. Some cross-reactivity is seen with mammalian cytochrome p450 enzymes
Azoles – Pharmacodynamics
Concentration-independent fungistatic agents
Dosage escalation may be necessary when faced with more resistant fungal species (e.g. Candida glabrata)
Goal of dosing is to maintain AUC:MIC >50
i.e. maintain concentrations 1-2 x MIC for the entire dosing interval
The therapy of fungal infections, once limited and toxic, has undergone an explosive period of development in recent years. Since the middle of the 1990s, new agents with novel mechanisms of action, enhanced potency, improved pharmacokinetics, and substantially less toxicity have reached the marketplace. The lipid amphotericin B formulations extended the life of this valuable agent by reducing its notable toxicity. The azole group of compounds has provided excellent alternatives to amphotericin B in the treatment of most clinically important mycoses. Research into the development of newer antifungal agents that focused on novel targets yielded the echinocandins, which are the first new class of compounds in several decades. This class provides another alternative in the treatment of candidiasis and aspergillosis. With all the choices, clinicians must be cognisant of differences in the spectrum of activity, pharmacokinetics and drug interaction potential of antifungal agents so that they may select the most appropriate drug for their patient. In addition, antifungal drug resistance is also becoming increasingly recognized as an important clinical problem. Azole resistance, especially to fluconazole, has been frequently reported. As more antifungal agents become available, drug resistance will likely continue to be a problem. Further advances in antifungal chemotherapy will be necessary to improve management of invasive mycoses in the future.
The discovery of new molecular targets in both yeasts and filamentous fungi that will render these organisms susceptible to novel antifungal drugs is likely to continue in view of the major challenge by systemic fungal infections in clinical medicine today.
Also, we need to learn more about combination antifungal therapy, e.g. about the effects of sequential blockade at two or more sites, and about the combination of antifungal agents with cytokines in an attempt to augment the inflammatory and immune responses of patients.
This overview of new antifungal drug development reflects the increased interest in this field of infectious diseases and demonstrates that, although some progress has been made, further efforts are necessary to develop more promising agents against invasive fungal disease.